Anuj Sharma MA1, Jenine Leal PhD2,3,4, Joseph Kim MD2, Craig Pearce MSc2, Dylan R. Pillai MD, PhD5, Aidan Hollis PhD1
1Department of Economics, University of Calgary, Calgary, Alberta, Canada.
2Infection Prevention and Control, Alberta Health Services, Calgary, Alberta, Canada
3Departments of Community Health Sciences and Microbiology, Immunology and Infectious Diseases, University of Calgary, Calgary, Alberta, Canada
4O’Brien Institute for Public Health, University of Calgary, Calgary, Alberta, Canada
5Departments of Pathology & Laboratory Medicine, Medicine, and Microbiology & Infectious Diseases, University of Calgary, Calgary, Alberta, Canada
Corresponding Author:
Aidan Hollis, Department of Economics, University of Calgary, Calgary, Alberta, Canada
Tel: 1-403-220-5861 | Email: ahollis@ucalgary.ca
ABSTRACT
Background: There is a need for robust estimates of per hour cost of contact precautions in hospitals. Our study aims to formulate and apply a methodology for estimating this cost.
Methods: A formula was established with components including patient room entries by Healthcare Worker (HCW), proportion of entries by HCW categories, time taken to don and doff Personal Protective Equipment (PPE), price of PPE, and HCW employment cost. A literature review for the period 2000-2020 was conducted to estimate room entries per hour; we applied proportion of room entries reported in literature; a local study was used for estimating time taken to don and doff gown and gloves; the price of PPE was provided by Alberta Health Services; and employment cost was captured from public sources.
Results: Results of the literature review suggest an average 4.35 entries per hour by HCW and most entries were made by nurses. The local study data suggested that on average it took 85 seconds in total for HCW to don and doff PPE. Using all the components of the formula, the total cost per hour per patient associated with additional PPE was estimated to be C$8.95 (US$6.82).
Conclusion: A simple framework for estimating hourly costs of contact precautions was presented. Although the hourly cost was modest, the implications are significant when considering annual number of patient-hours of contact precautions.
KEYWORDS
Contact precautions, PPE, cost
INTRODUCTION
With the recent development of many rapid diagnostic tests for infection, hospitals are facing challenging questions about which ones to implement [1,2]. One potential benefit of rapid tests is allowing the early discontinuation of contact precautions where appropriate. Contact precautions are used in hospitals with an aim to reduce the transmission of pathogens, including antibiotic-resistant organisms [3]. While shown to be effective in limiting pathogen transmission in hospital settings, implementing contact precautions can also add cost burden related to additional use of personal protective equipment (PPE) and designated isolation rooms [4-6]. Most studies on costs associated with PPE for any contact precautions have used a random average or proxy for number of room entries to determine the number of PPE used per isolation day/hour [6-10]. Contact precautions require little PPE, with patients on droplet or airborne precautions needing additional (and more costly) PPE.
The objective of this study was to formulate and apply a methodology for estimating the cost per hour of contact precautions. An accurate estimation of additional costs associated with contact precautions may enable better assessment of the financial benefit from appropriate early discontinuation. The methodology may be extended to address costs of other isolation regimens, such as those required for airborne precautions.
METHODS
In this study, we estimated the time and material cost associated with the use of gowns and gloves for contact precautions. We do not consider other potentially associated costs, such as private accommodation or additional cleaning.
To estimate all costs of keeping a patient on contact precautions, there are multiple components requiring assessment. These can be summarized as C=E×(T×∑iFiWi+P), where E represents the number of room entries per hour, T the time it takes to don and doff gown and gloves, Fi the fraction of each type of Healthcare Worker (HCW) among all room entries, Wi the hourly employment cost of each type of HCW, and P the price of gown and gloves. We therefore estimate each of these components separately and then calculate the total estimated cost per hour of contact precautions C. All dollar values are shown in 2020 Canadian dollars.
Patient Room Entries (E)
Search strategy and study selection
Literature search strategies (detailed in the Appendix) were each formulated for EMBASE and PubMed abstract databases, and all articles published on or before March 28, 2020 were included. There was no restriction imposed on the language of the articles.
In this literature review, inclusion criterion was defined as all articles that studied HCW or personal visitor entries to isolated patient rooms as compared to non-isolated patient rooms in a hospital. The exclusion criterion was defined as the absence of reported mean room entries for isolated patient rooms.
The study selection procedure was independently performed by two authors (AS and AH) in two phases. Firstly, screening of titles and abstracts were done based on the inclusion criterion. In the second phase, an independent manual review of the full text of these articles was conducted based on the exclusion criterion.
Data extraction and synthesis
The selected studies were utilized to obtain data points independently by two authors (AS and AH). These data points included study designs, reasons for isolation precautions, population characteristics, data collection period, data collection time of the day, type of room entries included, room type, number of patients in isolated and/or non-isolated groups, and mean patient room entries and p-values.
Statistical analysis and estimations
All analysis was performed using Microsoft Excel. Mean number of room entries per hour per patient along with p-values of test of the difference between isolated and non-isolated groups from studies selected in literature review were tabulated.
Time to Don and Doff Gown and Gloves (T)
Local study for time to don and doff PPE at
Foothills Medical Centre, Calgary, Canada
The data was originally collected as part of a Quality Improvement (QI) project. The objective of this study was to remove additional precautions for a set of patients (those colonized with Vancomycin-Resistant Enterococci and no other risk factors). Volunteer data collectors were trained by one author (CP) to time and record donning and doffing. They sat at the end of a hallway and, for 1 hour, recorded each time an HCW entered the room. Volunteers collected information on time taken by HCWs to don and doff gown and gloves, not including time for hand hygiene. HCWs were distinguished by their clothing types.
Statistical analysis and estimations
All analysis was performed using Microsoft Excel. Mean time to don and doff gown and gloves from the local study data were calculated and tabulated. Estimated time to don and doff gown and gloves from the local study were compared with a tutorial video posted by Public Health Ontario.
Proportion of Room Entries by HCW from the Literature (F)
For data on the proportion of room entries by HCW, we used articles that reported such proportions from our literature review of patient room entries. We used the average of the proportions from the shortlisted articles.
Mean employment cost of HCW from Open-Source Website (W)
Mean hourly wage rate of HCW categories, including doctors, nurses and housekeeping staff in Canada was abstracted from https://www.salaryexpert.com. To calculate employment costs, we grossed up wages to account for non-salary benefits, using the same proportions of salary to non-salary benefits as those shown in Schedule 2 of the 2020 Alberta Health Services Annual report for each category of HCW. This allowed us to calculate the hourly employment costs.
Cost of Gown and Gloves (P)
Cost of gown and gloves used for contact precautions in hospitals was collected from Alberta Health Services. The cost of laundering a gown was $0.42 and cost of purchasing a pair of nitrile gloves was $0.10.
RESULTS
Room Entries: Literature Review
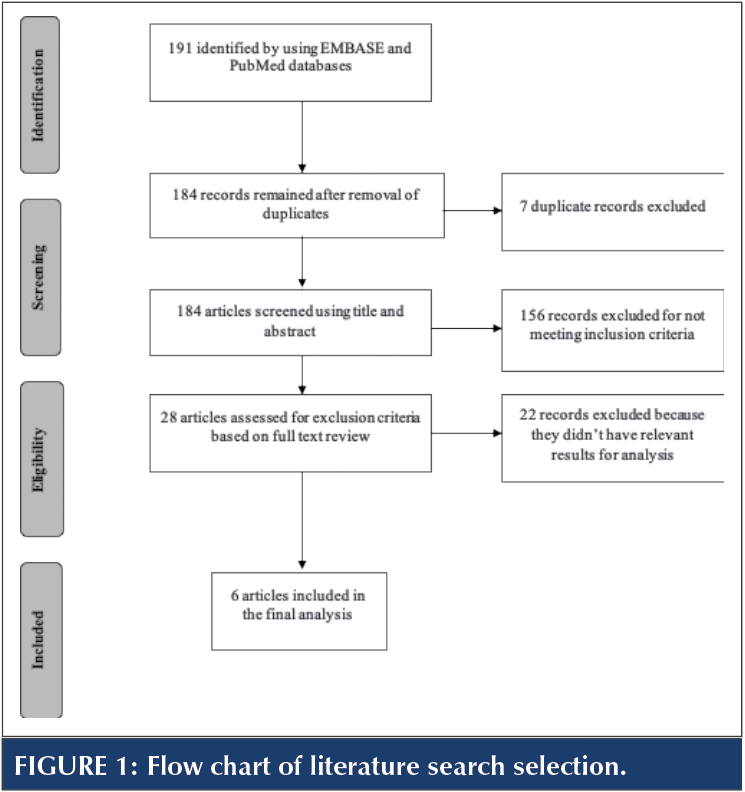 The flow of the literature search selection process was depicted in Figure 1. There were 191 literature abstracts found on EMBASE and PubMed. There were seven duplicates found and removed. Out of the remaining 184 articles, 156 were excluded in the first screening of titles and abstracts because they did not meet the inclusion criteria. This left 28 articles for the full-text screening based on the exclusion criterion. Only six out of these publications had relevant results for analysis.
The flow of the literature search selection process was depicted in Figure 1. There were 191 literature abstracts found on EMBASE and PubMed. There were seven duplicates found and removed. Out of the remaining 184 articles, 156 were excluded in the first screening of titles and abstracts because they did not meet the inclusion criteria. This left 28 articles for the full-text screening based on the exclusion criterion. Only six out of these publications had relevant results for analysis.
A summary of the studies which had relevant results for analysis was presented in Table 1. The studies included observational, quasi-experimental, case control and randomized controlled trial designs, which included both children and adult populations. All but one study examined the impact of contact precautions for antibiotic-resistant organisms. Data collection period in terms of total hours of room entry observations was greater than 490 hours in all but one study with a range of 91 to 10,080 hours [12]. There were two studies that collected entry data using electronic monitors, which allowed observation for a full 24 hours of the day [13,14]. Other studies collected only day and evening time data [12,15-17]. All studies recorded HCW visits and three studies included personal visitors. Most studies included both Intensive Care Unit (ICU) and Non-ICU wards, and one study included an Intermediate Care Unit (IMCU).
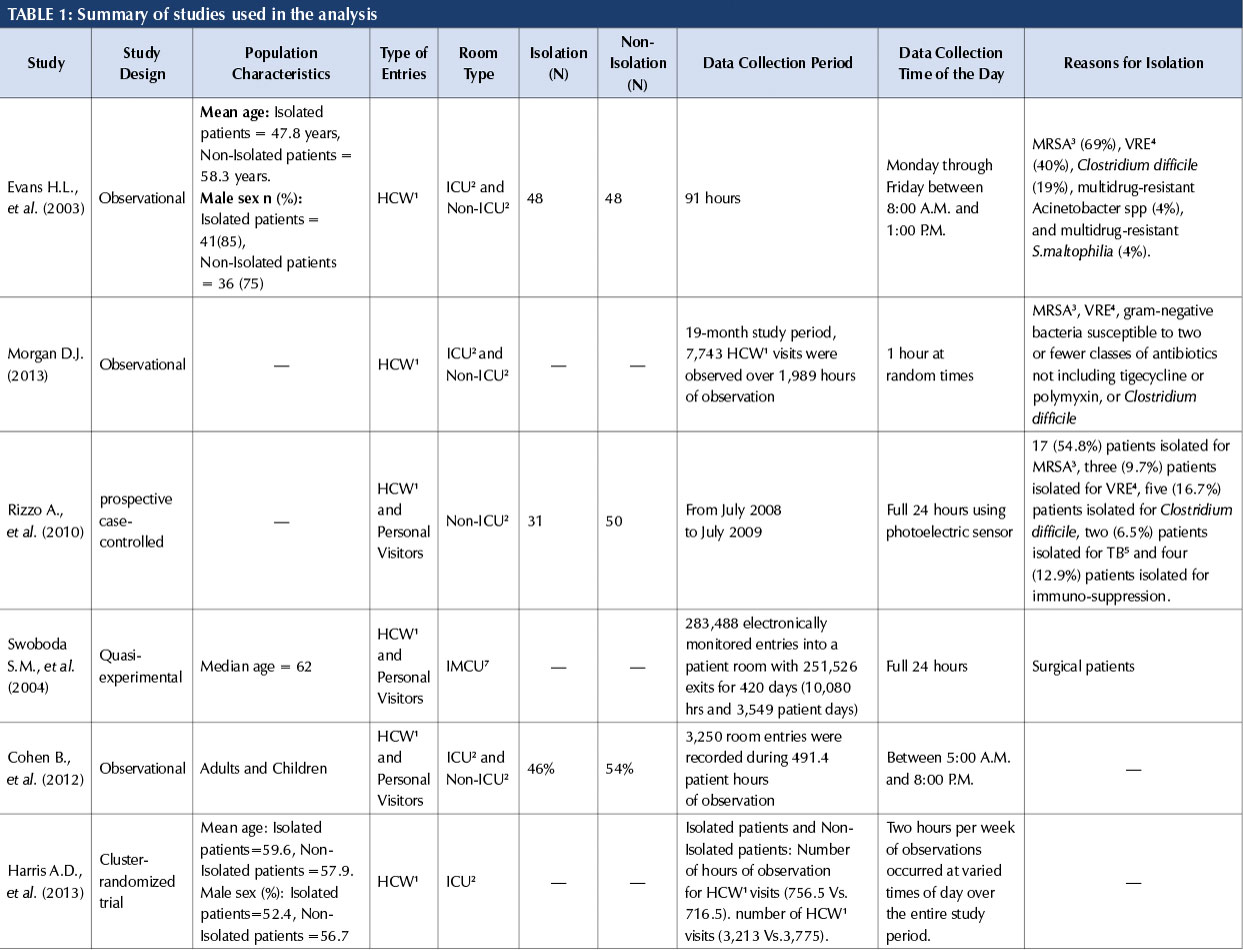
Note: 1Healthcare Workers; 2Intensive Care Unit; 3Methicillin-resistant Staphylococcus aureus; 4Vancomycin-Resistant Enterococci; 5Tuberculosis
Mean Room Entries from Literature Review
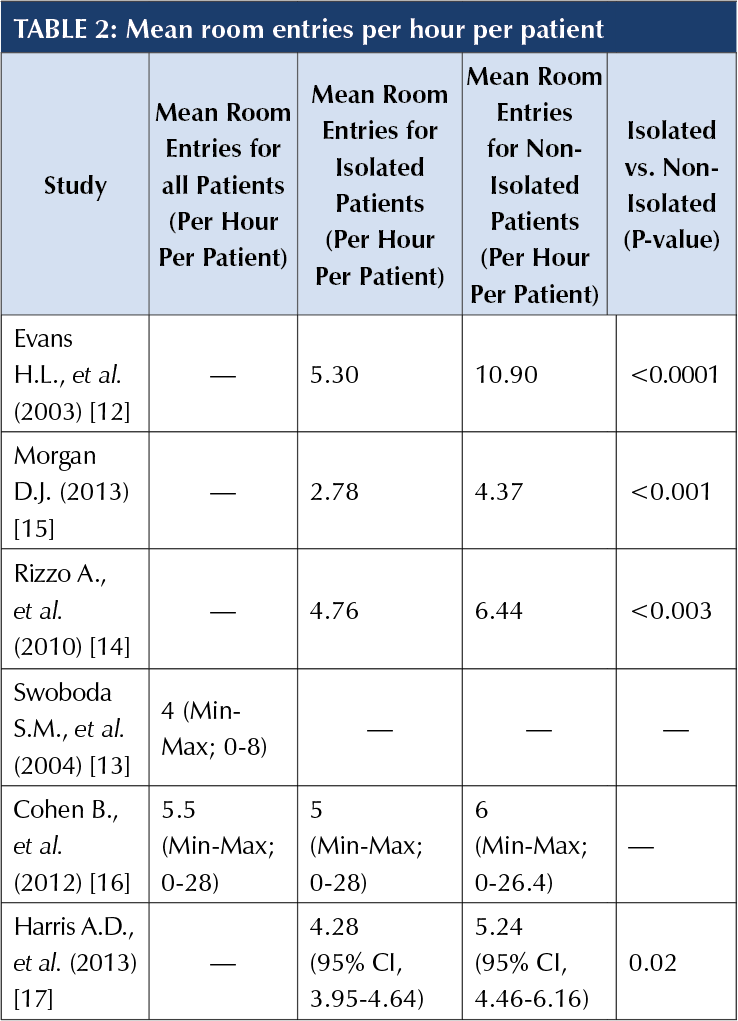 The mean room entries reported in the selected studies are presented in Table 2, and ranged from 2.78 to 5.3 per hour per patient for isolated patients and from 4.37 to 10.90 per hour per patient for non-isolated patients. In general, HCW entered more in non-isolated patient rooms than the isolated rooms and this difference was statistically significant.
The mean room entries reported in the selected studies are presented in Table 2, and ranged from 2.78 to 5.3 per hour per patient for isolated patients and from 4.37 to 10.90 per hour per patient for non-isolated patients. In general, HCW entered more in non-isolated patient rooms than the isolated rooms and this difference was statistically significant.
For the purpose of cost estimation, we used the average of the mean number of entries into isolated patient rooms from five studies and mean number of entries into all patient rooms from one study. (Since the latter was almost equal to the mean number for isolated patients, removing it would not have any effect on our estimates [13].) This average was 4.35 entries per hour per patient. We did not differentiate between ICU and non-ICU patients, since there was no clear pattern of differences in the number of entries.
Time to Don and Doff PPE from Local Study
The analysis from the QI study presented in Table 3 showed that on an average, it took 56.07 seconds for HCW to don gown and gloves and 28.92 seconds to doff gown and gloves. We examined the tutorial videos for how to don and doff gown and gloves posted by Public Health Ontario (https://www.youtube.com/watch?v=6YybqhkIL9M and https://www.youtube.com/watch?v=sk4A96IW8bQ). The examples in these videos take 68 (41) seconds to don (doff) gown and gloves, slightly longer than the means from the QI study. There are a few cases in the QI study in which HCWs took much longer than the mean to don or doff gowns and gloves, in which case, it is possible that the HCWs were involved in some other activity – such as a conversation – at the same time. We have not attempted to adjust for this formally.
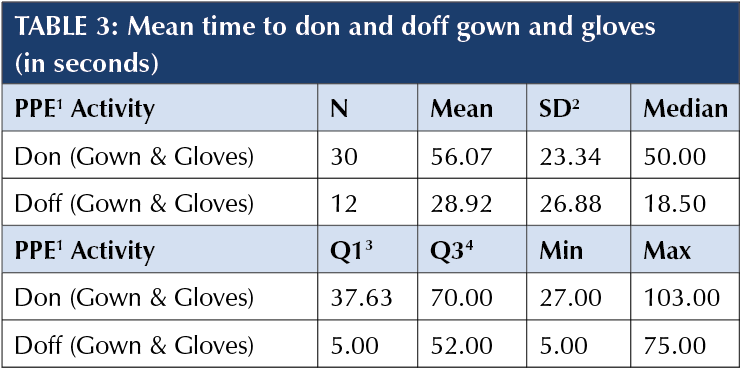
Note: PPE: 1Personal Protective Equipment; SD: 2Standard Deviation; Q1: 3First quartile; Q3: 4Third quartile.
Proportion of Room Entries by HCW Categories
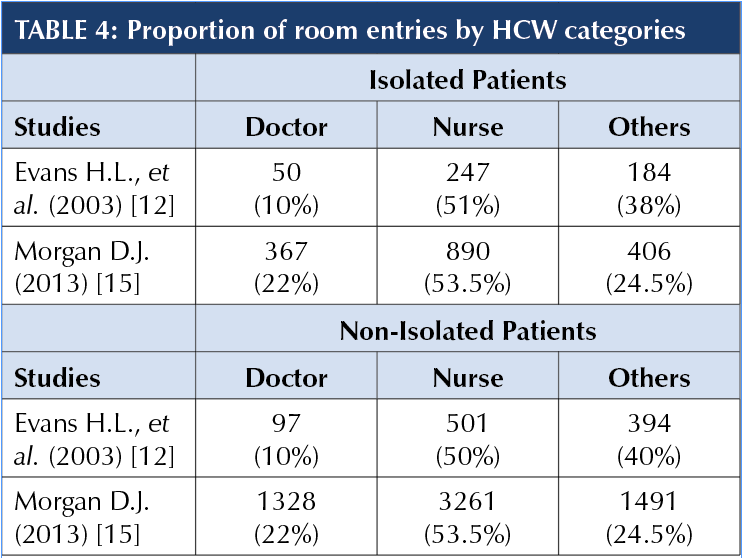 Three studies reported a breakdown of room entries by HCW categories [12,15,16]. Of these, two studies that reported proportions by isolated and non-isolated patient groups were used [12,15]. These studies categorized HCW into three broad types i.e., nurses, doctors and others. Others included hospital housekeeping staff.
Three studies reported a breakdown of room entries by HCW categories [12,15,16]. Of these, two studies that reported proportions by isolated and non-isolated patient groups were used [12,15]. These studies categorized HCW into three broad types i.e., nurses, doctors and others. Others included hospital housekeeping staff.
The proportion of entries by HCW categories in the literature presented in Table 4 showed that the majority of patient room entries was made by nurses, followed by others and doctors. The average proportion of patient room entries in the isolated patient rooms by HCW categories from these two studies was calculated as 16% for doctors, 53% for nurses and 31% for others.
Mean wage rate of HCW Categories
Table 5 shows the mean hourly wage and employment cost in Canada for hospitalists, nurses and others (hospital housekeepers). The non-salary benefits were 49.5% for physicians, 33% for nurses, and 24% for other staff.
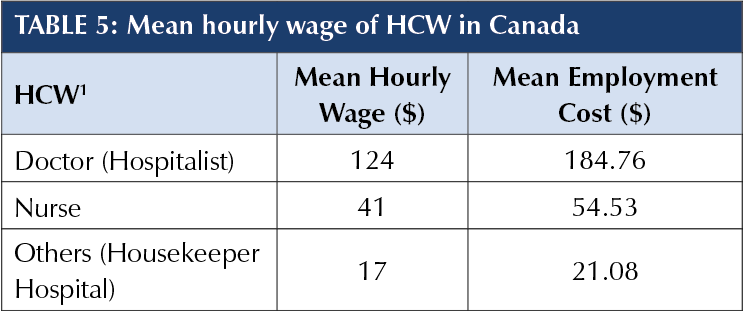
Note: 1Healthcare Workers
Source: https://www.salaryexpert.com; https://www.salaryexpert.com/salary/job/hospitalist/canada; https://www.salaryexpert.com/salary/job/nurse/canada; https://www.salaryexpert.com/salary/job/housekeeper-hospital/canada
Summary of PPE Costs Attributed to Contact Precautions
The total-per-hour cost associated with additional PPE was $8.76 (Table 6). The chief component in total cost was the labour cost of HCW related to time required for donning and doffing PPE, which was estimated to be $6.49. The estimated daily cost of contact precautions was $210 (or US$150). Table 6 presents point estimates, allowing each element of the cost to be adjusted based on specific circumstances, such as the cost per gown, the number of room entries, or the employment cost per hour.
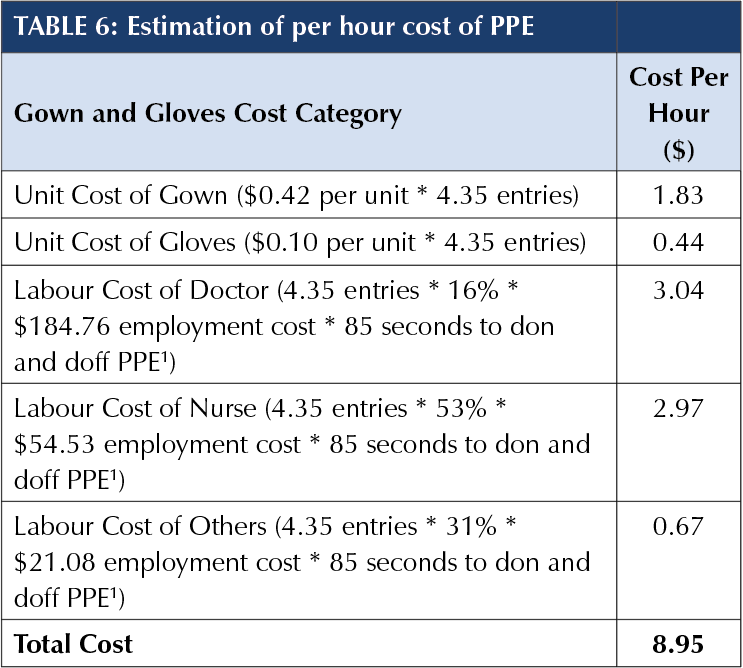
Note: 1Personal Protective Equipment
DISCUSSION
This study combines data on room entries from existing studies with data on time to don and doff gown and gloves from a QI study, along with specific data on employment costs and PPE costs, within a transparent framework to estimate the hourly cost of contact precautions. Results from the literature review on patient room entries suggests that HCWs, on average, entered isolated patient rooms 4.35 times in an hour and most of these entries were made by nurses (53%) followed by others (31%) and doctors (16%). Estimates from the local QI study imply that it takes HCWs 85 seconds to don and doff gown and gloves on average. This time is shorter than in the Ontario demonstration videos we examined, which may be intentionally slow to clarify the steps required. Using these numbers along with average hourly wage rate of HCWs in Canada, our study estimated that the per-hour cost of gown and gloves attributed to contact precautions was approximately $8.95.
The approach that we have used, with accurately reported room entries from published literature and new data on time to don and doff gown and gloves, gives our estimates a high degree of credibility. In addition, our study allows hospitals or researchers to apply components of our costing (e.g., number of room entries per hour) mixed with other location-specific components (e.g., salaries) to obtain estimates of additional cost of contact precautions. Similarly, the formula may be applied in other settings, such as long-term care facilities, where contact precautions are applied, with appropriate adjustments. The formula used in our study can also be easily extended to other types of isolation precautions. There may be other costs related to additional precautions, which were not included in our calculation. For example, a previous study estimated per-day costs of anxiety and depression in terms of quality adjusted life-year (QALYs) at approximately US$9.83 [18]. These costs can be used to evaluate cost-benefit analysis of implementing rapid diagnostic tests for infectious diseases.
Existing studies on the cost of contact precautions in terms of use of gown and gloves have a large range of estimates from as low as US$14.40 (accounting for materials only) to as high as GBP300 per day [5-10]. The estimated cost of contact precautions examined in this study falls in the middle at approximately $210 (US$153) per day.
Unnecessary additional precautions may be costly. In order to evaluate the added value of rapid diagnostic tools that may aid in timely discontinuation of isolation precautions, accurate estimation of costs associated with isolation precautions is imperative. While the estimated cost per hour was modest, given the number of hours of contact precautions, the implications are not insubstantial. For example, an analysis of VA hospitals in the US reported that within 8,318,675 patient-days during the years 2007-2010, about 13.6% were for patients with MRSA on contact precautions, which approximates 27 million hours [19]. At Foothills Medical Centre in Calgary, Alberta, internal data show that the proportion of patients on contact precautions has varied from 5% to 10% over the years 2014-2019. However, it is also important to acknowledge that not applying contact precautions, or terminating them too early, may also be costly and harmful to patients, depending on the specific circumstances [4].
While we have focused on the dollar cost of contact precautions, another perspective on contact precautions is that compliance requires significant time. If unnecessary contact precautions are lifted, HCWs will have additional time to devote to patient care. As we show above, HCWs spend about 6 minutes in donning and doffing gowns and gloves for every hour that patients are on contact precautions.
Our study has many limitations. There was variability in population characteristics of the studies used in the literature review on patient room entries. Additionally, only two of the reviewed studies counted room entries over the entire 24-hour period. All other studies focused on daytime hours only and therefore would capture only the busiest time for room entry. The sample size of the local study on time to don and doff gown and gloves was small with considerable variation, and compliance with PPE varies by location. We did not account for the difference between ICU and other wards. Also, we did not include any post-hospital discharge enhanced terminal cleaning specific to contact precautions as our focus was on the effect of shortening or extending contact precautions.
In conclusion, our study provides a simple framework to estimate the hourly costs of contact precautions, which may be used and adapted by other healthcare settings using local information on practices and costs. Future studies should consider mechanisms to improve the measurement of entries into isolation and non-isolation rooms, by different healthcare workers, over a 24-hour period.
FUNDING ACKNOWLEDGEMENT
The authors gratefully acknowledge support from Canadian Institutes of Health Research, grant 389455.
APPENDIX
Literature search strategy: EMBASE and PubMed
EMBASE = (‘infection’:ab,ti OR ‘infections’:ab,ti OR ‘infectious’:ab,ti OR ‘contagion’:ab,ti OR ‘contagious’:ab,ti) AND (‘hospital’:ab,ti OR ‘hospitals’:ab,ti OR ‘inhospital’:ab,ti OR ‘in-hospital’:ab,ti OR ‘hospitalization’:ab,ti OR ‘hospitalisation’:ab,ti OR ‘hospitalized’:ab,ti OR ‘hospitalised’:ab,ti OR ‘inpatient’:ab,ti OR ‘in-patient’:ab,ti) AND (‘isolation’:ab,ti OR ‘quarantine’:ab,ti OR ‘contact precaution’:ab,ti
OR ‘contact precautions’:ab,ti) AND (‘room entry’:ab,ti
OR ‘room entries’:ab,ti OR ‘ward entry’:ab,ti OR ‘ward entries’:ab,ti OR ‘visit’:ab,ti OR ‘visits’:ab,ti) AND (‘human’/de)
PubMed = (((((isolation[Title/Abstract] OR quarantine[Title/Abstract]) OR contact precautions[Title/Abstract]) OR contact precaution[Title/Abstract] OR patient contact[Title/Abstract]) AND (hospital[Title/Abstract] OR hospitals[Title/Abstract] OR inhospital[Title/Abstract]) OR in-hospital[Title/Abstract]) OR hospitalization[Title/Abstract] OR hospitalisation[Title/Abstract] OR hospitalised[Title/Abstract] OR hospitalized[Title/Abstract] OR inpatient[Title/Abstract] OR in-patient[Title/Abstract]) AND (infection[Title/Abstract] OR infections[Title/Abstract] OR infectious[Title/Abstract]) OR contagion[Title/Abstract] OR contagious[Title/Abstract] AND ( (ward[Title/Abstract] OR room[Title/Abstract]) AND (entry[Title/Abstract] OR entries[Title/Abstract])OR (hcw [Title/Abstract] and visit[Title/Abstract]) OR (hcw [Title/Abstract] and visits[Title/Abstract]) OR (healthcare worker[Title/Abstract] and visit[Title/Abstract]) OR (healthcare worker[Title/Abstract] and visits[Title/Abstract]) ) AND “humans”[MeSH Terms]
REFERENCES
1. Sexton ME, Jacob JT. (2017). Optimal use of rapid diagnostics in infection control and prevention. Clinical Microbiology Newsletter, 39, 83–89.
https://doi.org/10.1016/j.clinmicnews.2017.05.001.
2. Sullivan K V., Bard JD. (2019). New and novel rapid diagnostics that are impacting infection prevention and antimicrobial stewardship. Current Opinion in Infectious Diseases, 32, 356–364. https://doi.org/10.1097/QCO.0000000000000565.
3. Siegel JD, Rhinehart E, Jackson M, Linda; Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings (2007) 2019:1–204.
4. Sprague E, Reynolds S, Brindley P. (2016). Patient isolation precautions: Are they worth it? Canadian Respirology Journal, 2016, 1–5. https://doi.org/10.1155/2016/5352625.
5. Jan A. Roth, MD; Claudia Hornung-Winter PIR. (2018). Direct costs of a contact isolation day: A prospective cost analysis at a Swiss university hospital. Infection Control and Hospital Epidemiology, 39, 9–11.
6. Verlee K, Berriel-Cass D, Buck K, Nguyen C. (2014). Cost of isolation: Daily cost of isolation determined and cost avoidance demonstrated from the overuse of personal protective equipment in an acute care facility. American Journal of Infection Control, 42, 448–449.
https://doi.org/10.1016/j.ajic.2013.10.014.
7. Spence MR, Dammel T, Courser S. (2012). Contact precautions for methicillin-resistant Staphylococcus aureus colonization: Costly and unnecessary? American Journal of Infection Control, 40, 535–538. https://doi.org/10.1016/j.ajic.2011.07.016.
8. Hübner C, Hübner N-O, Muhr M, Claus F, Leesch H, Kramer A, et al. (2015). Cost analysis of hospitalized Clostridium difficile-associated diarrhea (CDAD). GMS Hygiene and Infection Control, 10,Doc13. https://doi.org/10.3205/dgkh000256.
9. Kunori T, Cookson B, Roberts JA, Stone S, Kibbler C. (2002). Cost-effectiveness of different MRSA screening methods. Journal of Hospital Infection, 51, 189–200. https://doi.org/10.1053/jhin.2002.1247.
10. Otter JA, Burgess P, Davies F, Mookerjee S, Singleton J, Gilchrist M, et al. (2017). Counting the cost of an outbreak of carbapenemase-producing Enterobacteriaceae: an economic evaluation from a hospital perspective. Clinical Microbiology and Infection, 23, 188–196.
https://doi.org/10.1016/j.cmi.2016.10.005.
11. Alberta Health Services, Consolidated Financial Statements, March 31, 2020. Retrieved from
https://www.albertahealthservices.ca/assets/about/publications/ahs-pub-2019-20-financials.pdf, accessed 23 October 2020.
12. Evans HL, Shaffer MM, Hughes MG, Smith RL, Chong TW, Raymond DP, et al. (2003). Contact isolation in surgical patients: A barrier to care? Surgery, 134,
180–188. https://doi.org/10.1067/msy.2003.222.
13. Swoboda SM, Earsing K, Strauss K, Lane S, Lipsett PA. (2004). Electronic monitoring and voice prompts improve hand hygiene and decrease nosocomial infections in an intermediate care unit. Critical Care Medicine, 32, 358–363. https://doi.org/10.1097/01.CCM.0000108866.48795.0F.
14. Rizzo A, V. Trivedi, T. Aldaghlas, R. Richmond, R. Sun LR. Care for the Isolation Patient: Not enough? Assoc Acad Surg Soc Univ Surg 2010.
15. Morgan DJ, Pineles L, Shardell M, Graham MM, Mohammadi S, Forrest GN, et al. (2013). The effect of contact precautions on healthcare worker activity in acute care hospitals. Infection Control and Hospital Epidemiology, 34,69–73. https://doi.org/10.1086/668775.
16. Cohen B, Hyman S, Rosenberg L, Larson E. (2012). Frequency of patient contact with health care personnel and visitors: Implications for infection prevention.
Joint Commission Journal on Quality and Patient Safety, 38, 560–565. https://doi.org/10.1016/S1553-7250(12)38073-2.
17. Harris AD, Pineles L, Belton B, Johnson JK, Shardell M, Loeb M, et al. (2014). Universal glove and gown use and acquisition of antibiotic-resistant bacteria in the ICU.
Survey of Anesthesiology, 58, 158–159.
https://doi.org/10.1097/sa.0000000000000059.
18. Sharma A, Pillai DR, Lu M, Doolan C, Leal J, Kim J, et al. (2020). Impact of isolation precautions on quality of life: a meta-analysis. Journal of Hospital Infection, 105, 35-42. https://doi.org/10.1016/j.jhin.2020.02.004.
19. Jain R, Kralovic SM, Evans ME, Ambrose M, Simbartl LA, Obrosky DS, et al. (2011). Veterans Affairs initiative to prevent nethicillin-resistant Staphylococcus aureus infections. New England Journal of Medicine. 364, 1419–1430.
https://doi.org/10.1056/NEJMoa1007474.



