Sachin Pasricha, MD1; Chantal R. Valiquette, MD1; Megan Singh, MD1; Rohini Pasricha1; Darwin Jimal1;
Faiza Khurshid, MD, FCPS, Msc1,2
1 Queen’s University School of Medicine; Kingston, Ontario, Canada.
2 Department of Pediatrics, Kingston Health Sciences Centre; Kingston, Ontario, Canada.
Corresponding author:
Sachin Pasricha, MD
Kingston Health Sciences Center
Watkins 3, Room 4 3 218
76 Stuart Street
Kingston, ON K7L 2V7
spasricha@qmed.ca
ABSTRACT
Background: Given nosocomial infections remain a prominent issue in the Neonatal Intensive Care Unit (NICU), this quality improvement study aimed to observe adherence to the NICU Moments of Hand Hygiene (MHH) and Bare Below the Elbow (BBE) guidelines, identify barriers to adherence, and propose solutions for improving adherence.
Methods: Investigators observed and statistically compared adherence (using an N-1 chi-squared test and two-tailed p <0.05 representing significance) of Healthcare Practitioners (HCPs) in the NICU to the MHH and BBE guidelines for 24 one-hour shifts, stratifying by moment, body part, participant role, and time. HCPs and families completed questionnaires to identify adherence barriers. Questionnaire and observational data underwent qualitative thematic analysis to identify potential barrier solutions.
Results: Moment 1A (before contact with the environment outside the patient’s isolette) adherence of (51%) was lowest and significantly different than adherence to Moments 1B (before entering the isollette) (66%, p<0.05), moment 3 (after potential body fluid exposure) (81%, p=0.02), and moment 4 (upon leaving the care environment) (60%, p=0.01). Nursing MHH adherence (61%) was significantly better than medical staff/trainee (38%) (p=0.002) and family member adherence (44%) (p=0.02).
Forearm BBE adherence (53%) was lowest and statistically different from wrist (85%), hand/finger (91%), and nail (96%) adherence (all p=0.01). Daytime (82%) and nighttime (73%) BBE adherence were significantly different (p=0.006). A majority of providers identified skin irritation, forgetfulness, and busy environment as MHH barriers, and lacking a secure jewelry location and forgetfulness as BBE barriers, while almost all family members found hand hygiene equipment to be available and constantly filled.
Conclusions: MHH adherence differs by moment and participant role, and BBE adherence differs by body part and time, justifying targeted interventions. Strategies such as secure jewelry storage, better temperature regulation in the unit, more hand lotion, and improved signage may improve adherence.
KEYWORDS: Neonatology, Infection Control, Hand Hygiene, Quality Improvement
INTRODUCTION
Nosocomial infections are a prominent issue for hospitals and patients [1, 2], particularly in the Neonatal Intensive Care Unit (NICU), where infection rates can be as high as 25% [3, 4],
reflecting inherent patient vulnerability from exposure to invasive procedures. Neonatal nosocomial infections are associated with adverse outcomes, including prolonged hospitalization, morbidity, and mortality [5, 6].
Hand hygiene is a globally recognized best practice in infection prevention and control [7]. The World Health Organization (WHO) and Public Health Ontario guidelines suggest implementing institutional multifaceted hand hygiene programs to ensure compliance [7, 8]. Adhering to the Moments of Hand Hygiene (MHH) and providing alcohol-based hand rub at point of care is essential, but remains challenging. Ontario’s Provincial Infectious Diseases Advisory Committee (PIDAC) issued the 2015 perinatology best-practice guideline, which divides the neonatal and immediate neonatal care environments, thereby establishing an extra MHH on entry to the isolette/warmer (i.e., there were five NICU MHH) in Ontario. These five moments of hand hygiene include:
1A) before contact with the immediate care environment (including the monitors, machines, chart, and outside the isolette), 1B) before contact with the neonatal environment (inside the isolette), 2) before an aseptic procedure, 3) after
potential body fluid exposure, and 4) after leaving the immediate care environment. The PIDAC guidelines also stress the importance of being Bare Below the Elbow (BBE) (i.e., no bracelets, rings, or watches should be worn in the provision of direct neonatal patient care) [9]. This is because white coats, rings, and artificial nails may potentially harbor microorganisms [10-12].
Adherence to the PIDAC best practice guidelines reduces NICU nosocomial infection [13]. For example, studies suggest that a target of 80% hand hygiene adherence can translate to a nosocomial infection rate of one infection per 100 patient days in the NICU [14], justifying audit and feedback initiatives to improve guideline adherence. According to the United States Joint Commission, there are three ways to audit adherence: direct observation, measuring product use, and survey questionnaires [15]. In Ontario, the “Just Clean Your Hands” campaign provides a tool to audit adherence [8]. However, this tool is not equipped to observe the NICU microsystem and its additional MHH. The absence of the additional 1B moment on auditing tools prevents us from understanding how well the five MHH are adhered to. To our knowledge, there is no published literature that addresses how well the five MHH and BBE practices are followed in Canadian NICUs. Moreover, there is limited information regarding barriers specific to NICU hand hygiene, which is important because hand hygiene is a behavioural practice; understanding barriers can translate into the development of positive reinforcement techniques, which promote long-lasting attitude changes [16].
The present study employs direct observation and questionnaires, as suggested by the Joint Commission, to address this gap in the literature [15]. The specific objectives are to 1) Observe adherence to the PIDAC’s 2015 MHH and BBE guidelines in a Canadian NICU, 2) Survey Healthcare Providers (HCPs) and families to reveal their perceptions of performing hand hygiene and adherence behaviors, and 3) Propose solutions towards improving adherence.
METHODS
Study Design
This cross-sectional study took place from March 4 to August 27, 2018 in the NICU. It consisted of direct observation and questionnaires.
Setting
The Kingston Health Sciences Centre NICU is a 24-bed level II/III
care facility that sees approximately 400 admissions per year. Hospital hand hygiene audits are part of routine accreditation reports mandated by the provincial Ministry of Health.
The NICU-specific results are reviewed by a nursing manager quarterly. The present study’s observations took place outside of the regular audits.
Institutional Review Board
The study was approved by the KHSC Research Ethics Board. The Project was completed with the assistance of hospital administration allowing direct observation.
Observation
Personnel: HCPs and patient families were directly observed. HCPs included trainees, nurses, physicians, respiratory therapists, and those not providing direct care, but accessing the environment (e.g., maintenance staff). Of note, though patient families are not universally trained in hand hygiene, they do get an abbreviated hand-hygiene training in our NICU and were therefore observed.
Data Collection: Five observers (S.P., C.V., M.S., R.P., D.J.), whom are medical students or resident physicians and were trained by the study’s supervising investigator who specializes in quality improvement, performed one-hour mock observation and discussed what actions constitute violating adherence, so as to reduce interobserver variability. The observers individually observed on weekdays and weekends for 24 one-hour shifts (13 day shifts between 07:00 and 19:00 hours, and 11 night shifts between 19:00 and 07:00 hours). Two shifts, maximum, were performed per day. Observation periods intentionally overlapped with nurse handover, meals, and family visitation. Investigators used an adapted version of the “Just Clean Your Hands” campaign observational tool to record moments of adherence and non-adherence to both the MHH and BBE guidelines during these observational periods [8]. Observers recorded only adherence and non-adherence events that were directly witnessed. The adapted observation tool also had designated space for qualitative comments.
Questionnaire
Recruitment: For the HCP questionnaire, an email was distributed to 60 NICU nurses/allied health professionals and 20 neonatologists/pediatric residents through Qualtrics, an online survey platform, with the link to study details and questionnaire. Inclusion was based upon providing consent through Qualtrics, which was voluntary. The email was re-sent at two weeks and four weeks following the initial email. For a six-week period, the patient family questionnaire was printed and distributed to every patient family member if the patient’s stay was more than seven days, as these family members are likely to spend a significant amount of time in the NICU. This included 40 families. Participation was voluntary and returning a completed questionnaire was considered implied consent. A record sheet was maintained to avoid duplicate entries.
Questionnaire Content: The HCP questionnaire included three demographic questions, five knowledge questions, and 23 Likert scale items to assess perceived adherence barriers. The knowledge assessment portion of the HCP questionnaire was adapted from a guide to improve hand hygiene by the Institute for Healthcare Improvement [17]. The patient family questionnaire included four demographic questions and 15 Likert scale items to assess attitudes and perceived barriers that could not be directly observed. The Likert scale questions were derived from literature review [13-16].
Data Analysis
Observation: The MHH adherence rate was stratified by the five moments, participant role (e.g., doctor, nurse, family member), and time (e.g., day, night). The BBE adherence rate was stratified by body part (e.g., hand/finger, wrist, and forearm), participant role, and time. Based on these stratifications, adherence was statistically compared with an N-1 chi-squared test with a two-tailed alpha of 0.05 [18]. Verbatim observer comments were collated to inform qualitative analysis, but are, however, not reported as a separate component of this study.
Questionnaire: Results were reported descriptively. That is the number and percentage of respondents that answered each question with a specific item. Demographic and knowledge-based questions were treated as categorical data and Likert scale items as ordinal data.
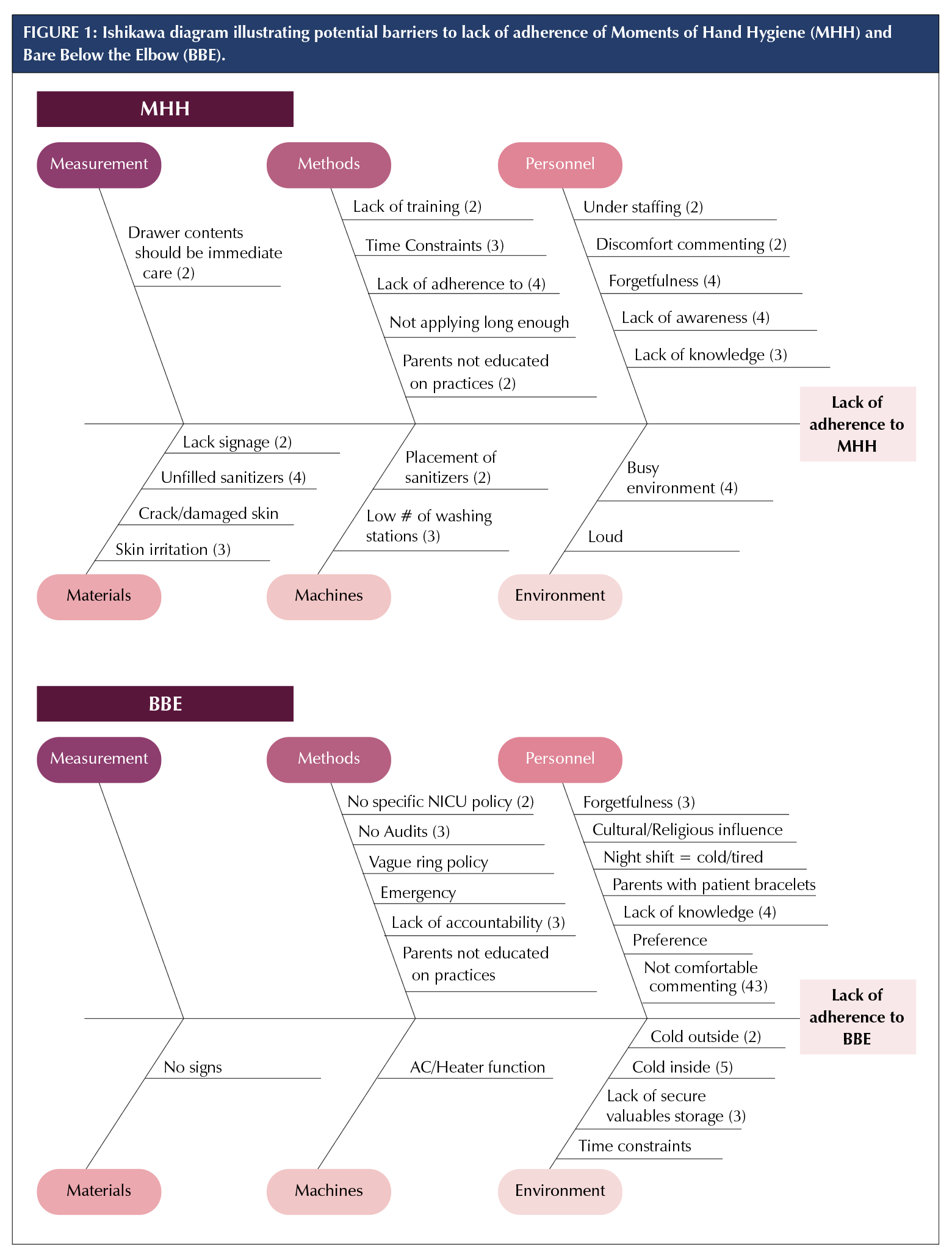
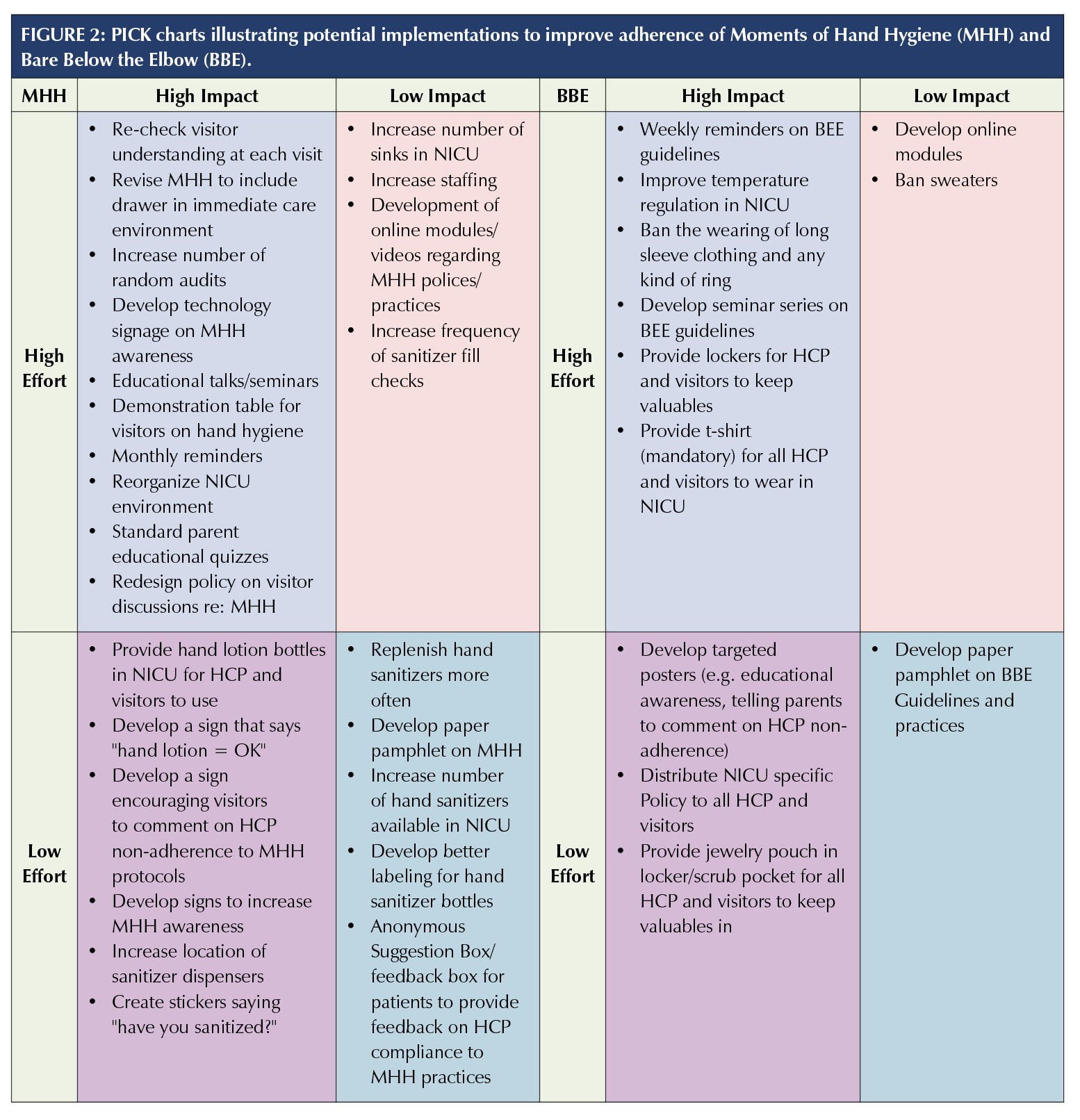
Thematic analysis: Qualitative thematic analysis was performed using an inductive approach. Five reviewers (S.P., C.V., M.S., R.P., and D.J.) reviewed the observation and questionnaire results to independently identify barriers to adherence to the MHH and BBE guidelines and place these barriers on Ishikawa diagrams (fishbone diagrams that attempt to discern the cause of an event that are commonly used in quality improvement studies) [19]. The reviewers then independently proposed solutions to poor adherence and graphed them on two PICK (Possible, Implement, Challenge, and Kill) charts (2x2 table that categorizes solutions to a problem based on payoff and difficulty) [20]. Each chart reflected potential interventions to increase adherence to the MHH and BBE guidelines respectively. The five reviewers then collaborated using the independently created Ishikawa diagrams and PICK charts to create two cumulative Ishikawa diagrams and two cumulative PICK charts (one for MHH and one for BBE respectively), and then decide upon three most optimal MHH and BBE-related interventions.
RESULTS
Observation
Overall, MHH adherence was 59% (571/974). Moments 1A and 2 were least adhered to (51% and 50%, respectively). There was a statistically significant difference between Moment 1A adherence compared with 1B (66%, p<0.05), 3 (81%, p<0.05), and 4 adherence (60%, p=0.01) (Table 1). Additionally, we found Moment 3 was the most adhered to (81%). There was a statistically significant adherence difference between Moment 3 compared with 1A, 2, and 4 (p=<0.05 for all three). When comparing participant role, there was a statistically significant difference between medical staff/trainee (38%) and nurse/nursing trainee adherence (61%, p=0.002), as well as family member (44%) and nurse/nursing trainee adherence (p=0.02), though the number of observations for medical staff/trainees (45) and families (43) were less than for nurse/nursing trainees (830).
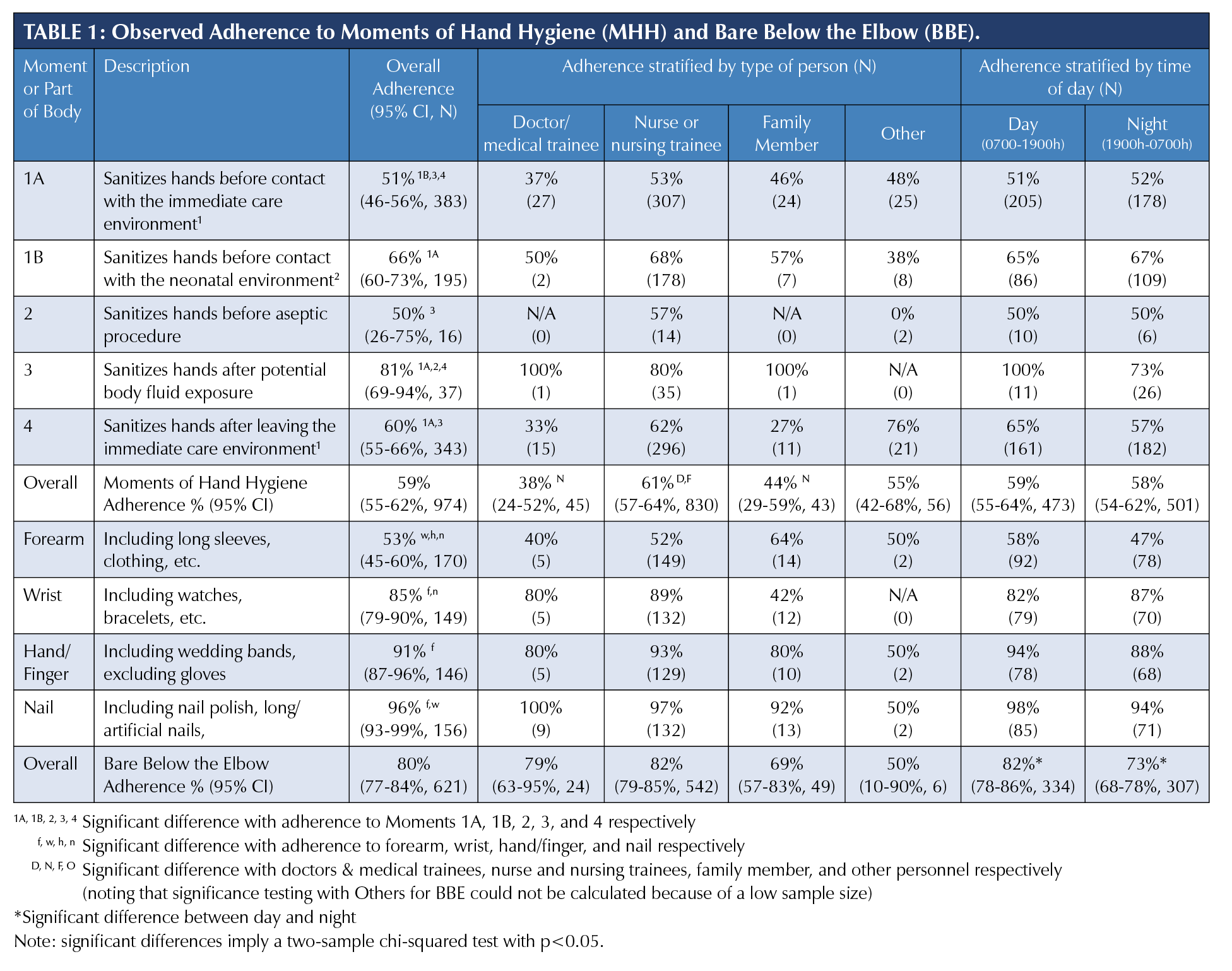
Overall, BBE adherence was 80% (499/621). Forearm adherence was least common (53%), with a statistically significant difference compared with wrist (85%), hand/finger (91%), and nail (96%) adherence (all p<0.05). There was also a statistically significant difference between nighttime (73%) and daytime BBE adherence (82%) (p=0.006).
Questionnaire
Twenty-four of 60 HCPs (40% response rate) completed the entire online questionnaire, which included two of 10 medical staff/trainees (20%) and 21 of 60 nurses/nursing trainees/allied healthcare personnel (35%). Of note, not every respondent answered every question. Twenty-six of 40 patient families (65%) completed the questionnaire.
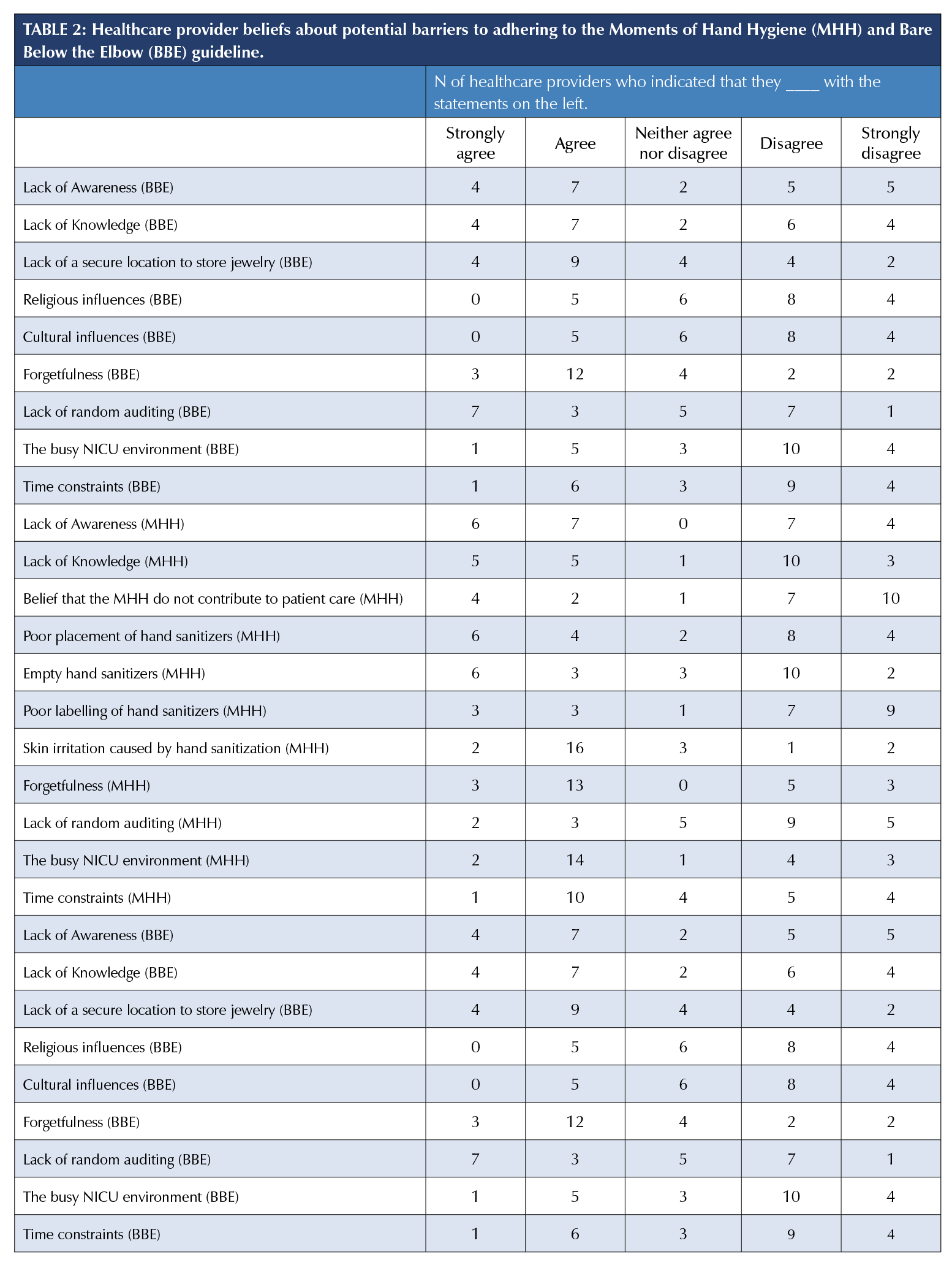
With respect to the HCP questionnaire, 18 of 24 (75%) respondents indicated skin irritation, 16 of 24 (67%) indicated forgetfulness, and 16 of 24 (67%) indicated the busy NICU environment as barriers (Table 2). A total of 15 of 23 (65%) respondents agreed or strongly agreed that forgetfulness and 13 of 23 (57%) agreed or strongly agreed that the lack of a secure location to store jewelry and other valuables are barriers to adhering to the BBE guideline. Of note, five of 23 (22%) respondents disagreed or strongly disagreed that they or other HCPs are comfortable commenting on witnessed failure to adherence to MHH/BBE guidelines.
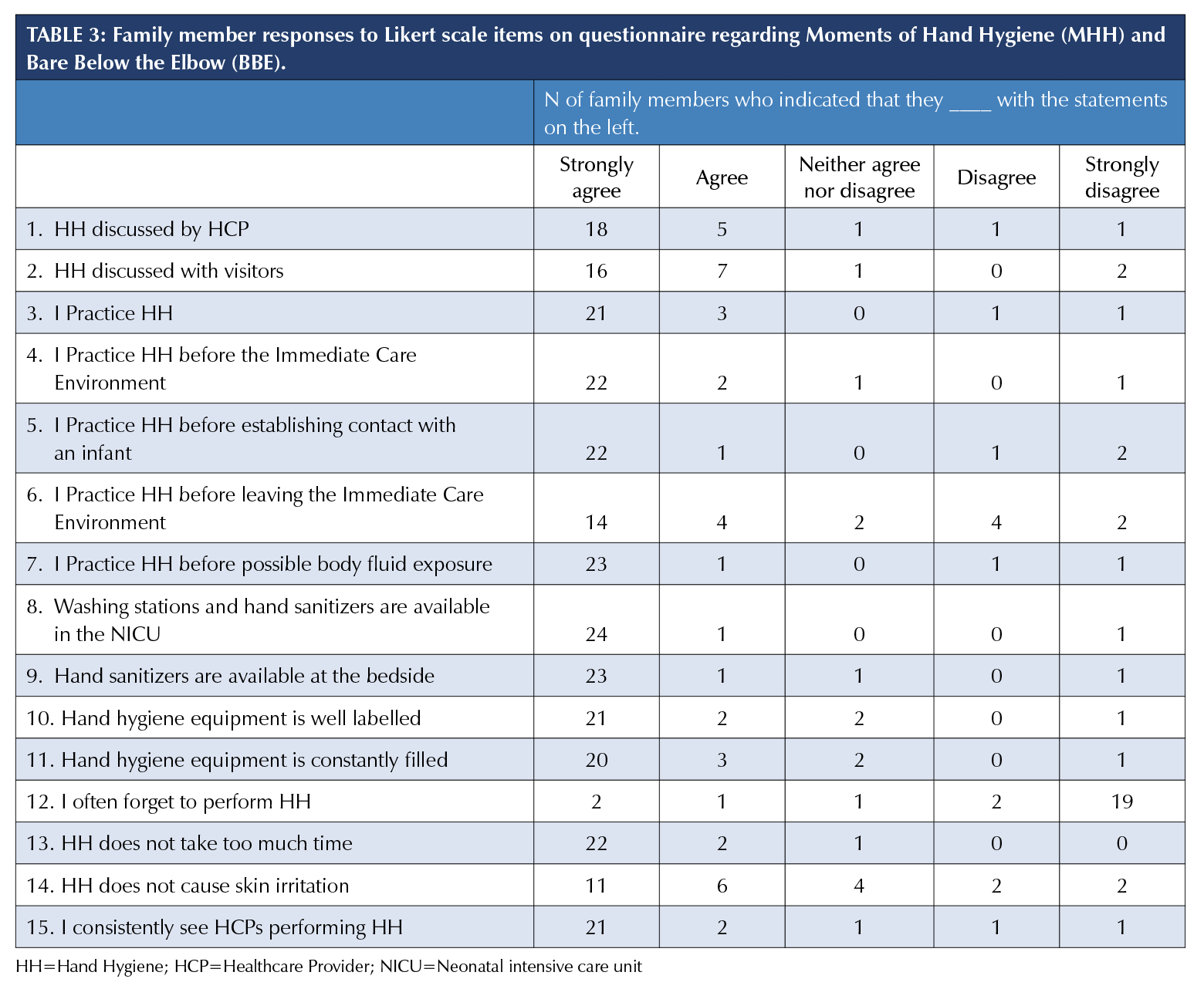
With respect to the patient family questionnaire, the majority of respondents agreed or strongly agreed that hand hygiene equipment is available in the NICU (25 respondents, 96%), at the bedside (24 respondents, 92%), is well labelled (23 respondents, 88%) and is constantly filled (23 respondents, 88%) (Table 3).
Qualitative Thematic Analysis
The collaborative data analysis process conducted by investigators resulted in Ishikawa diagrams (Figure 1) that identified barriers to MHH and BBE adherence. The most commonly identified MHH barriers were lack of awareness, forgetfulness, and unfilled sanitizers (each identified by four of five reviewers), followed by time constraints, lack of knowledge, skin irritation, and lack of washing stations (each identified by three of five). The most commonly identified BBE barriers were cold temperatures (identified by five of five reviewers), lack of knowledge (identified by four of five), forgetfulness, lack of accountability, lack of auditing, and the fact that parents are uncomfortable commenting about HCP non-adherence (each identified by three of five). The PICK charts identified potential implementations that could improve adherence as depicted in Figure 2. The three most optimal MHH-related implementations were: placing hand lotion in the NICU alongside signage that using it to alleviate skin irritation is permitted, improving parent education, and improving overall MHH signage. The three optimal BBE-related implementations were: a poster targeted at rolling up your sleeves, improving temperature regulation, and having secure pouches to store jewelry.
DISCUSSION
This study evaluated hand-hygiene adherence according to PIDAC’s NICU-specific MHH and BBE guidelines and identified resource-efficient solutions that may improve adherence. Among the MHH, adherence varied widely by moment and provider, with Moment 1A and 2 least adhered to, Moment 3 most adhered to, and nursing staff having better adherence than medical staff. As for the BBE guideline, adherence varied by body part and time, with forearm adherence least common and daytime adherence better than nighttime. Identified solutions to improving adherence included hand lotion stations, improved signage, a secure jewelry location, and improved temperature regulation.
The primary aim of the study was to observe adherence to NICU hand-hygiene guidelines. Prior literature describes that NICU MHH adherence may be as high as 79% [21], and routine audit data provided by the KHSC NICU ranged from 80-90% in previous fiscal years. Conversely, our study found an overall adherence rate of only 59%. Our study adds to the literature by directly addressing PIDAC recommendations and providing a stratified analysis of MHH and BBE adherence, whereas most prior studies and routine hospital audits do not. Our study sheds light on five specific findings. First, we found that adherence to Moments 1A, 1B, 2, and 4, and forearm adherence to the BBE guideline are all below 80%, which is an important threshold that seems to correspond with an infection rate of 1 infection per 100 NICU patient days [14]. Second, Moment 1B was more adhered to than Moment 1A, suggesting that HCPs may be more cognizant of interactions with the neonate than surrounding equipment. Third, Moment 3 was the only moment with greater than 80% adherence, which may be due to visible soiling of hands after body fluid exposure serving as a reminder to complete hand hygiene or the routine of completing hand hygiene after removal of Personal Protective Equipment which is used during potential body fluid exposures. Fourth, our analysis supports evidence from prior studies that suggest nurses/nursing trainees have better adherence than doctors/medical trainees [22]. Finally, with respect to the BBE guidelines, forearm and nighttime adherence were low, often due to HCPs wearing sweaters at nighttime. Wearing sweaters below the elbows is important to identify and avoid because hospital uniforms carry significant amounts of bacteria [23].
Another aim of the study was to identify adherence barriers and resource-efficient quality improvement solutions. Prior studies suggest that skin irritation caused by hand sanitization is a barrier, and this resulted in the suggestion of hand lotion dispensers throughout hospitals [24]. Educational tools, such as teaching modules, explicit training sessions, and signage, have also been suggested to be effective [25-27]. Our study supports the idea that hand lotion and reminder signage may improve adherence in our institution. Our study adds to the aforementioned literature by identifying that a secure jewelry location and improved temperature regulation of the NICU in general may improve adherence. Moreover, parents reported discomfort with speaking up about witnessed non-adherence; whether this results from the busy NICU culture demands further investigation [28]. Some prior studies do suggest that having parents and patients speak up about hygiene non-adherence may prove to be a more sustainable solution than one-off educational reminders [29].
This study is not without limitations. First, there was no formal measure of intra- or inter-rater reliability. An initial mock observation shift and use of qualitative observations with periodic observer discussions were conducted to limit inter-rater reliability. As well, HCPs and parents may have been aware of observation efforts, creating a Hawthorne effect. In addition, this study proposes interventions but does not implement them or assess their actual effectiveness. Finally, the low response rate for the HCP questionnaire (29%) may cause non-response bias. Future studies might see a better response rate with various questionnaire administration modalities
(e.g., web-based, mobile-based, and in-person), shorter survey length, and survey completion incentives.
Despite these limitations, our study has three primary strengths. First, it signifies the difference between routine hand
hygiene audits versus environment and workplace-specific
audits. One crucial finding was that adherence to MHH 1A and 1B were both low. Though not explicitly identified in our observation or questionnaires, it is important to acknowledge how low adherence may trigger guideline creators like PIDAC to reconsider the boundaries of the neonatal and immediate care environments. Another strength was including patient families. Our study adds perspective to the limited existing literature, which includes visitor data and interventions for hand hygiene [29-32]. This is important as NICUs have transitioned to a family-integrated care methodology, where families provide direct care beyond just skin to skin [30].
A final strength is that data was collected from researchers who were not part of the clinical team, so they could observe and provide thematic analysis without bias.
Overall, hand-hygiene adherence varied widely by moment and provider for the MHH, and body part and time for the BBE guideline, suggesting value in targeted interventions. Notably, nursing staff had better MHH adherence than medical staff. This study supports certain interventions identified by prior literature (e.g., hand lotion stations and improved signage), while proposing new interventions (e.g., secure jewelry location and improved temperature regulation of the NICU in general) that can inform future quality improvement efforts.
REFERENCES
1. Plowman R, Graves N, Griffin MA, Roberts JA, Swan AV, Cookson B, et al. The rate and cost of hospital-acquired infections occurring in patients admitted to selected specialties of a district general hospital in England and the national burden imposed. J Hosp Infect. 2001;47(3):198-209. doi: 10.1053/jhin.2000.0881.
2. Revelas A. Healthcare-associated infections: A public health problem. Niger Med J. 2012;53(2):59-64. doi: 10.4103/0300-1652.103543.
3. Liu J, Sakarovitch C, Sigurdson K, Lee HC, Profit J. Disparities in Health Care-Associated Infections in the NICU. Am J Perinatol. 2020;37(2):166-73. doi: 10.1055/s-0039-1688481.
4. Rogowski JA, Staiger D, Patrick T, Horbar J, Kenny M, Lake ET. Nurse staffing and NICU infection rates. JAMA Pediatr. 2013;167(5):444-50. doi: 10.1001/jamapediatrics.2013.18.
5. Edwards JR, Peterson KD, Mu Y, Banerjee S, Allen-Bridson K, Morrell G, et al. National Healthcare Safety Network (NHSN) report: data summary for 2006 through 2008, issued December 2009. Am J Infect Control. 2009;37(10):783-805. doi: 10.1016/j.ajic.2009.10.001.
6. Polin RA, Denson S, Brady MT, Committee on F, Newborn, Committee on Infectious D. Epidemiology and diagnosis of health care-associated infections in the NICU. Pediatrics. 2012;129(4):e1104-9. doi: 10.1542/peds.2012-0147.
7. World Health Organization. WHO Guidelines on Hand Hygiene in Health Care: First Global Patient Safety Challenge Clean Care Is Safer Care. WHO Guidelines Approved by the Guidelines Review Committee. Geneva 2009.
8. Public Health Ontario. Just Clean Your Hands – Hospitals Toronto, Ontario.2019 [cited 2020]. Available from: https://www.publichealthontario.ca/en/health-topics/infection-prevention-control/hand-hygiene/jcyh-hospitals.
9. Best Practices for Infection Prevention and Control in Perinatology. Provincial Infectious Diseases Advisory Committee (PIDAC), Public Health Ontario, 2015. Available from: https://www.publichealthontario.ca/-/media/documents/b/2015/bp-ipac-perinatology.pdf?la=en
10. Treakle AM, Thom KA, Furuno JP, Strauss SM, Harris AD, Perencevich EN. Bacterial contamination of health care workers’ white coats. Am J Infect Control. 2009;37(2):101-5.
11. Trick WE, Vernon MO, Hayes RA, Nathan C, Rice TW, Peterson BJ, et al. Impact of ring wearing on hand contamination and comparison of hand hygiene agents in a hospital. Clin Infect Dis. 2003;36(11):1383-90.
12. McNeil SA, Foster CL, Hedderwick SA, Kauffman CA. Effect of hand cleansing with antimicrobial soap or alcohol-based gel on microbial colonization of artificial fingernails worn by health care workers Clin Infect Dis. 2001;32(3):367-72.
13. Pessoa-Silva CL, Hugonnet S, Pfister R, Touveneau S, Dharan S, Posfay-Barbe K, et al. Reduction of health care associated infection risk in neonates by successful hand hygiene promotion. Pediatrics. 2007;120(2):e382-90. doi: 10.1542/peds.2006-3712.
14. Won SP, Chou HC, Hsieh WS, Chen CY, Huang SM, Tsou KI, et al. Handwashing program for the prevention of nosocomial infections in a neonatal intensive care unit. Infect Control Hosp Epidemiol. 2004;25(9):742-6. doi: 10.1086/502470.
15. The Joint Commission. Measuring Hand Hygiene Adherence: Overcoming the Challenges. Akron, Ohio: 2009.
16. Hill S. A Behavior-Focused Hand Hygiene Quality Improvement Project. Nursing Graduate Publications and Presentations. 2016;8.
17. Institution for Healthcare Improvement. How-to Guide: Improving Hand Hygiene. Cambridge, MA, USA: 2006.
18. Stuart A OJ, Arnold S. Kendalls Advanced Theory of Statistics. 2A. London: Arnold; 1999. p. 17.
19. Hall Barber K, Schultz K, Scott A, Pollock E, Kotecha J, Martin D. Teaching Quality Improvement in Graduate Medical Education: An Experiential and Team-Based Approach to the Acquisition of Quality Improvement Competencies. Acad Med. 2015;90(10):1363-7. doi: 10.1097/ACM.0000000000000851.
20. Harel Z, Silver SA, McQuillan RF, Weizman AV, Thomas A, Chertow GM, et al. How to Diagnose Solutions to a Quality of Care Problem. Clin J Am Soc Nephrol. 2016;11(5):901-7. doi: 10.2215/CJN.11481015.
21. El-Kafrawy U, Taylor RJ, Francis N, Boussabaine E, Badrideen M. Effectiveness of a neonatal intensive care unit access intercom linked audiovisual display monitor highlighting infection control procedures. Am J Infect Control. 2013;41(8):749-50. doi: 10.1016/j.ajic.2012.10.021.
22. Allegranzi B, Gayet-Ageron A, Damani N, Bengaly L, McLaws ML, Moro ML, et al. Global implementation of WHO’s multimodal strategy for improvement of hand hygiene: a quasi-experimental study. Lancet Infect Dis. 2013;13(10):843-51. doi: 10.1016/S1473-3099(13)70163-4.
23. Sanon MA, Watkins S. Nurses’ uniforms: How many bacteria do they carry after one shift? J Public Health Epidemiol. 2012;4(10):311-5. doi: 10.5897/JPHE12.074.
24. Larson E, Girard R, Pessoa-Silva CL, Boyce J, Donaldson L, Pittet D. Skin reactions related to hand hygiene and selection of hand hygiene products. Am J Infect Control. 2006;34(10):627-35. doi: 10.1016/j.ajic.2006.05.289.
25. Mukerji A, Narciso J, Moore C, McGeer A, Kelly E, Shah V. An observational study of the hand hygiene initiative: a comparison of preintervention and postintervention outcomes. BMJ Open. 2013;3(5). doi: 10.1136/bmjopen-2013-003018.
26. Phan HT, Tran HTT, Tran HTM, Dinh APP, Ngo HT, Theorell-Haglow J, et al. An educational intervention to improve hand hygiene compliance in Vietnam. BMC Infect Dis. 2018;18(1):116. doi: 10.1186/s12879-018-3029-5.
27. Sadeghi-Moghaddam P, Arjmandnia M, Shokrollahi M, Aghaali M. Does training improve compliance with hand hygiene and decrease infections in the neonatal intensive care unit? A prospective study. J Neonatal Perinatal Med. 2015;8(3):221-5. doi: 10.3233/NPM-15915001.
28. Kirk J, Kendall A, Marx JF, Pincock T, Young E, Hughes JM, et al. Point of care hand hygiene-where’s the rub? A survey of US and Canadian health care workers’ knowledge, attitudes, and practices. Am J Infect Control. 2016;44(10):1095-101. doi: 10.1016/j.ajic.2016.03.005.
29. Naikoba S, Hayward A. The effectiveness of interventions aimed at increasing handwashing in healthcare workers - a systematic review. Journal of Hospital Infection. 2001;47(3):173-80.
30. Franck LS, Kriz RM, Bisgaard R, Cormier DM, Joe P, Miller PS, et al. Comparison of family centered care with family integrated care and mobile technology (mFICare) on preterm infant and family outcomes: a multi-site quasi-experimental clinical trial protocol. BMC Pediatr. 2019;19(1):469. doi: 10.1186/s12887-019-1838-3.


