Joanna Lo1; Yilei Luan1; Zerlyn Lee1; Lisa Jacques2; Lisa Krueckl2,3; Jocelyn A. Srigley4,5
1 Faculty of Medicine, University of British Columbia, Vancouver, Canada
2 BC Children’s Hospital, Vancouver, Canada
3 Vancouver Coastal Health, Squamish, Canada
4 Department of Pathology and Laboratory Medicine, BC Children’s Hospital and BC Women’s Hospital + Health Centre, Vancouver, Canada
5 Department of Pathology and Laboratory Medicine, University of British Columbia, Vancouver, Canada
Corresponding author:
Dr. Jocelyn Srigley
BC Children’s Hospital Microbiology Laboratory
4500 Oak Street, Room 2G9
Vancouver BC, V6H 3N1, Canada
Tel: 1-604-875-2000 ext. 5208
jocelyn.srigley@cw.bc.c
ABSTRACT
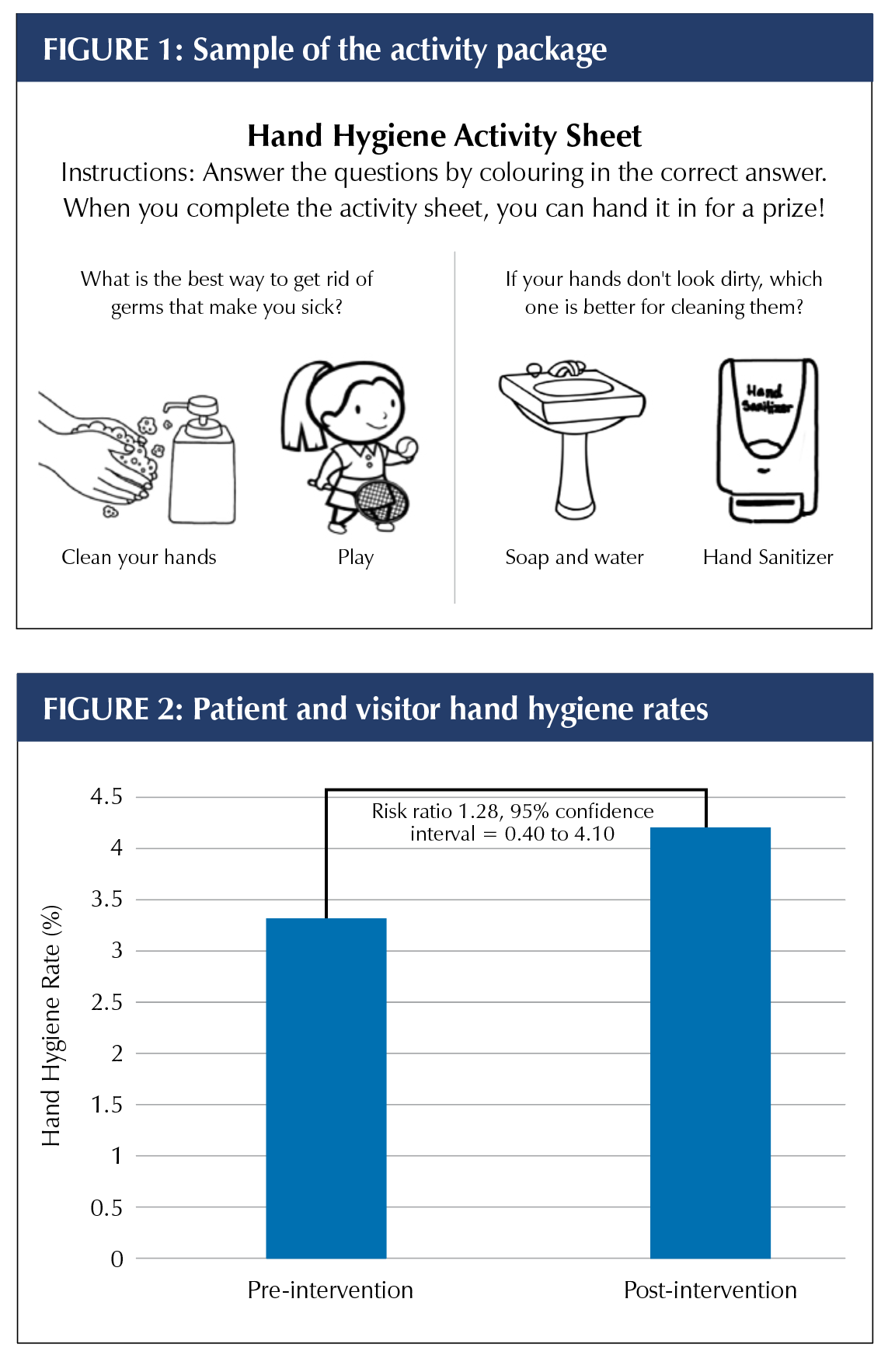
Patient and visitor hand hygiene (HH) interventions have been demonstrated to reduce the rate of healthcare-associated infections. Observational audits on the oncology/hematology/bone marrow transplant inpatient unit at British Columbia Children’s Hospital indicated that patient, family, and visitor HH was sub-optimal with a compliance rate of 3.3%. Despite creating interventions aimed at improving this, the post-intervention rate only increased to 4.2% (not significant, p>0.05). Future work will include investigating barriers to accessing and utilizing these resources.
KEYWORDS: Hand hygiene, paediatrics, quality improvement
INTRODUCTION
Paediatric oncology, hematology, and bone marrow transplant (BMT) patients are at high risk of acquiring healthcare-associated infections (HAIs), potentially resulting in significant morbidity and mortality. In a Canadian point prevalence survey of paediatric inpatients, 8% were found to have an HAI, with a trend towards increased risk among patients on hematology and oncology units [1].
Patients’ hands are frequently colonized with pathogens [2], and patient hand hygiene (HH) initiatives have been shown to decrease transmission of these pathogens [3]. However, patient and family/visitor HH is often overlooked as part of HAI prevention efforts [2-4]. Published studies have consistently reported sub-optimal patient HH rates [3], making it evident that this is an important target for quality improvement.
A baseline assessment conducted at our hospital revealed low patient, family, and visitor HH rates. In addition, only 38% of participants reported that healthcare workers (HCWs) had talked to them about HH, and 93% preferred soap and water to alcohol-based hand rub (ABHR) [5], despite ABHR being more effective and less irritating to hands than soap and water [6]. The objective of this project was to improve patient, family, and visitor HH rates through the use of nursing education and patient and visitor resources, which were designed to address the identified gaps.
METHODS
Study setting
This quality improvement project was conducted at the oncology/hematology/BMT unit at British Columbia Children’s Hospital (BCCH), the province’s tertiary, academic, acute care centre for paediatric patients. As determined by the Alberta Research Ethics Community Consensus Initiative (ARECCI) screening tool, a commonly used resource in many jurisdictions for assessing ethical considerations of projects, ethical approval was not required as this was a quality improvement project.
Data collection
Patient, family, and visitor HH rates were obtained through direct observation by three covert medical students who were trained according to provincial best practice guidelines [6], and used an electronic tool for anonymous data collection. Audit data were recorded according to the four moments of HH adapted for patients, families, and visitors by the BCCH Infection Prevention and Control team [7]. Baseline data were collected in May 2018, and post-intervention data were collected between April and May of 2019.
Development of hand hygiene interventions
Various interventions were designed by medical students, informed by results of a cross-sectional survey of patients and visitors on inpatient units at BCCH in 2018 [8,9]. The survey included both quantitative and qualitative responses designed to identify facilitators and barriers of HH. We also performed literature reviews, and held meetings with unit stakeholders to get their input. Three interventions were developed: an educational activity package for patients (Figure 1), an information pamphlet for adults (Appendix A) and a nursing checklist (Appendix A). Activities were created for different age groups, including comics, crosswords, word searches, and colouring pages. The nursing checklist contained key teaching points to be addressed with patients and visitors upon admission, including HH moments and use of ABHR.
Implementation of hand hygiene interventions
The interventions were implemented by the unit’s quality improvement lead and an infection control practitioner, who provided educational sessions over the course of four months to instruct nurses on how to use the checklists and materials developed for patients and families. Incorporation of HH education on existing checklists and provision of pamphlets in new diagnosis binders and admission packs were implemented in an effort to include HH education as part of standard teaching on the unit.
Data analysis
Quantitative audit data were compiled and HH rates were reported as a percentage for the time period prior to intervention implementation and the period during and following implementation. Chi square tests for significance were used to compare the rates.
RESULTS
There was a total of 302 HH observations made, with 251 being of visitors and 51 of patients. The overall HH rate prior to implementation of the interventions was 3.3% (Figure 2), with 183 observations made (six washes and 177 misses). In comparison, the post-intervention rate was 4.2% with a total of 119 observations (five washes and 114 misses). The difference between the two rates was non-significant (p-value=0.68).
DISCUSSION
Patient, family, and visitor HH was clearly sub-optimal in our project, consistent with the literature [3], and there are few interventions proven effective to improve HH in this population. Interventions used in other studies have been similar to the multimodal approach for improving HCW HH compliance, with provision of ABHR and education being the most common components [3]. Although other studies suggest that these interventions improved HH rates and decreased HAIs among patients, most of these studies had sub-optimal study design and heterogeneous outcomes [3]. Our prior work indicates that standard interventions such as posters and pamphlets are ineffective in increasing HH [7].
 Although HH increased post intervention, it remained low and lacked statistical significance. Barriers inhibiting the success of patient and family/visitor HH interventions must be identified and addressed. One potential issue in our project was the need to also take into account HCW behaviours and attitudes towards patient and family/visitor HH in order to develop more effective interventions. Although the interventions developed in our project were well-received by nurses at the educational sessions, sustained implementation of strategies and resources appeared to be limited. One way to approach this may be to more robustly involve nurses in the development of interventions through a frontline ownership approach to better understand what can be embedded within their existing workflows. Further insight could be obtained through the collection of feedback from nurses regarding their opinions around the resources already introduced. Interestingly, there was a perception among nurses that they were doing a good job of educating about HH despite survey data showing that the majority of patients/visitors did not recall hearing anything about HH from HCWs. This may be a good opportunity to utilize the teach-back method [10], to ensure patients/visitors understand the teaching and retain the information better.
Although HH increased post intervention, it remained low and lacked statistical significance. Barriers inhibiting the success of patient and family/visitor HH interventions must be identified and addressed. One potential issue in our project was the need to also take into account HCW behaviours and attitudes towards patient and family/visitor HH in order to develop more effective interventions. Although the interventions developed in our project were well-received by nurses at the educational sessions, sustained implementation of strategies and resources appeared to be limited. One way to approach this may be to more robustly involve nurses in the development of interventions through a frontline ownership approach to better understand what can be embedded within their existing workflows. Further insight could be obtained through the collection of feedback from nurses regarding their opinions around the resources already introduced. Interestingly, there was a perception among nurses that they were doing a good job of educating about HH despite survey data showing that the majority of patients/visitors did not recall hearing anything about HH from HCWs. This may be a good opportunity to utilize the teach-back method [10], to ensure patients/visitors understand the teaching and retain the information better.
The main limitation of this project is the before-after design. The lack of a control group limits the ability to determine cause and effect, although it is less relevant in this case since there was no change in hand hygiene post intervention. Second, process measures such as completion of the checklists were not included. Third, although the medical students who were performing HH observations received the same training, inter-rater reliability was not formally determined between them. Finally, generalizability of results to other settings and populations is not likely to be possible.
Future work should focus on barriers preventing nurses from providing HH education to patients and families/visitors, as well as seeking other innovative strategies to change behaviour. Conducting staff focus groups using a frontline ownership approach may help to improve uptake of the intervention and inform next steps. It would also be instructive to analyze the missed opportunities, as they may reveal barriers such as lack of, or inappropriate placement of ABHR dispensers, or gaps in knowledge regarding the moments of HH.
CONCLUSION
While much importance is placed on HCW HH to prevent HAIs within the oncology, hematology, and BMT setting, the focus needs to be broadened to include patient and family/visitor HH practices. Despite our interventions, HH rates continued to be low, indicating that re-evaluation and further innovation will be required to improve patient, family, and visitor HH rates.
REFERENCES
1. Rutledge-Taylor K, Matlow A, Gravel D, Embree J. A point prevalence survey of healthcare-associated infections in Canadian pediatric inpatients. Am J Infect Control 2012; 40(6): 491-496.
2. Hedin G, Blomkvist A, Janson M, Lindblom A. Occurrence of potentially pathogenic bacteria on the hands of hospital patients before and after the introduction of patient hand disinfection. Acta Path Micro IM C 2012; 120: 802-807.
3. Srigley JA, Furness CD, Gardam M. Interventions to improve patient hand hygiene: a systematic review. J Hosp Infect 2016; 94(1): 23-29.
4. Banfield KR, Kerr KG. Could hospital patients’ hands constitute a missing link? J Hosp Infect 2005, 61: 183-188.
5. Jacques L, Lee Z, Lo J, Luan Y, Krueckl L, Srigley JA. Oncology/hematology/BMT patient and visitor hand hygiene knowledge, attitudes, and practices [poster presentation]. The Association of Pediatric Hematology and Oncology Nurses, 43rd Annual Conference, San Jose, California, USA, 2019. http://3234439c809462d6446a-31b39e0745403b1c50ffafba111d4bac.r32.cf1.rackcdn.com/handouts/14P-OncologyHematologyBMT-Patient-and-Visitor-Hand.pdf
6. BC Ministry of Health. Best Practices for Hand Hygiene in All Healthcare Settings, http://www.health.gov.bc.ca/library/publications/year/2012/best-practice-guidelines-handhygiene.pdf; 2012 [accessed May 28, 2021].
7. Wong MWH, Xu YZ, Bone J, Srigley JA. Impact of patient and visitor hand hygiene interventions at a pediatric hospital: A stepped wedge cluster randomized control trial. Am J Infect Control 2020; 48: 511-516.
8. Lee Z, Lo J, Luan Y, Fernando J, Johannesen D, Masuda C, Swallow T, Srigley JA. Patient, family, and visitor hand hygiene knowledge, attitudes, and practices at pediatric and maternity hospitals: A descriptive study.
Am J Infect Control 2021; online ahead of print.
9. Smith JD, Corace KM, MacDonald TK, Febrigar LR, Saedi A, Chaplin A, MacFarlane S, Valickis D, Garber GE. Application of the theoretical domains framework to identify factors that influence hand hygiene compliance in long-term care. J Hosp Infect 2019; 101: 393-8.
10. Yen PH, Leasure AR. Use and effectiveness of the teach-back method in patient education and health outcomes. Fed Pract 2019;36(6):284-9.
Appendix A: Nursing Checklist
Date:
Patient, Family, and Visitor Hand Hygiene Checklist
Why are we teaching patients, families, and visitors about hand hygiene?
Patients, families, and visitors understand that hand hygiene is important, but they often do not know when or how they are supposed to clean their hands, especially in the hospital environment. In a survey conducted on the BCCH Oncology Inpatient unit in May 2018, only 14.3% of patients, families, and visitors reported that healthcare workers had spoken to them about hand hygiene. This could be due, in part, because education is often provided during the initial diagnosis which is a very stressful time for families and they may not hear or remember. Audit data also indicated that only 2.8% of patients, families, and visitors actually cleaned their hands when they were supposed to. Because of this low rate, it is important to educate patients, families, and visitors about the importance of hand hygiene in preventing the spread and acquisition of healthcare-associated infections, which kill 8,500-12,000 Canadian patients every year. This checklist and tools were developed to assist and standardize education provided to families and patients.
Patient and Visitor Hand Hygiene Education Checklist on Admission: