Reprinted with permission from the Official Journal of the Association of Medical Microbiology and Infectious Disease Canada.
Robert J Reid MD, PhD1,2, Laura Rosella PhD1,2, Natasha Milijasevic PhD1,3, Lorne N Small MD, MSc, FRCPC3,4
1Institute for Better Health, Trillium Health Partners, Mississauga, Ontario, Canada;
2Dalla Lana School of Public Health, University of Toronto, Toronto, Ontario, Canada;
3Trillium Health Partners, Mississauga, Ontario, Canada;
4Division of Infectious Diseases, Faculty of Medicine, University of Toronto, Toronto, Ontario, Canada
ABSTRACT
Background: The perceived risk of coronavirus disease 2019 (COVID-19) infection for healthcare workers (HCWs) is high. Although testing has focused on symptomatic HCWs, asymptomatic testing is considered by some to be an important strategy to limit occupational spread. Evidence on the results of large asymptomatic testing strategies in healthcare is, however, limited. This study examines the uptake and positivity of COVID-19 testing in a voluntary asymptomatic testing campaign at a large Canadian hospital.
Method: In addition to testing HCWs with symptoms, all asymptomatic staff were offered a COVID-19 test at Trillium Health Partners, a large Ontario hospital, from May 27 to June 15, 2020. Testing was offered in four waves, corresponding to the likelihood of exposure to COVID-19-positive patients. The mass asymptomatic testing campaign was offered when the hospital’s community test positivity rate had declined to 5%.
Results: Since March 16, the hospital has tested 51.3% of its 10,143-person workforce at least once. In the asymptomatic testing campaign for HCWs between May 27 and June 15, 27% of clinical and non-clinical staff received testing. No large differences were found in the proportions of clinical HCWs tested by their exposure to COVID-19-positive patients. In this campaign, 0.2% of asymptomatic HCWs tested positive. However, these individuals either had mild symptoms at testing and did not self-identify or became symptomatic after testing.
Conclusions: At this large hospital with declining community prevalence, a mass asymptomatic testing campaign of HCWs found they had a very low likelihood of testing positive for COVID-19.
KEYWORDS: asymptomatic, campaign, COVID-19, hospital, testing, workers
BACKGROUND
The human toll from coronavirus disease 2019 (COVID-19) continues to escalate worldwide [1]. With no effective vaccine available, pandemic control has focused on implementing public health measures to reduce transmission, as well as on case identification, isolation, and timely contact tracing.
A main goal has been to flatten the epidemic curve, prevent resurgences, and reduce stresses on hospitals and healthcare workers (HCWs). Public concern in Canada and across the world has been high, with HCWs perceiving their personal risk as significant, in part because of the increased risk of exposure and concerns about the availability of personal protective equipment (PPE) [2-7]. Some very limited evidence suggests that case rates may be higher among HCWs than among the general population, but the absolute risk varies with general community incidence and health system capacity [8,9]. The case rate differences between HCWs and the general public may also reflect higher levels of testing for HCWs [10]. In Ontario, HCWs account for approximately 5,327 (16%) of all confirmed cases, with most working in long-term-care homes and hospitals [11]. Some researchers have found that HCW risk varies by professional group and healthcare setting (e.g., COVID-19
hospital wards), but others have found no discernable differences among groups [8, 12, 13].
There have been many debates regarding optimal testing strategies for the general public and for HCWs specifically. Some experts promote mass testing of all HCWs to reduce occupational spread from atypical, mild, or asymptomatic cases, and to enable ongoing surveillance to protect the healthcare workforce over time [14]. Others argue that the harms outweigh the benefits, particularly with laboratory testing constraints [15] Limited studies, however, have examined the results of HCW testing strategies that include asymptomatic persons. In one study in a large, London-based National Health Service trust, serial testing of a sample of 400 asymptomatic HCWs revealed positive tests between 7.1% and 1.1% of staff in consecutive weeks on the downslope of the epidemic curve [16]. Another UK study found a 3.0% positivity rate among asymptomatic HCWs [17]. To our knowledge, no studies have reported uptake of testing and disease occurrence among asymptomatic HCWs in Canada. To fill this gap, this article examines a voluntary mass asymptomatic testing campaign for all HCWs at one of Canada’s largest community hospitals.
METHODS
Serving the Region of Peel in Ontario, Canada, Trillium Health Partners (THP) is a large, full-service hospital system with more than 1,300 inpatient beds, 9,700 clinical and back-office employees, and more than 1,300 affiliated physicians. In Ontario,
lockdown was announced on March 17, with case-doubling rates peaking around April 15 and slower growth after April 26. During this time, THP applied a variety of pandemic management strategies, including stopping elective surgeries, expanding PPE use, cohorting patients, and restricting visitors. On May 19, the province announced phased reopening. According to the Public Health Agency of Canada, at the time of writing, Ontario had 32,370 COVID-19 cases, accounting for 33% of all cases in Canada [18]. Peel is one of the most populous regions in Ontario (1.38 million), representing 10% of the provincial population. At the time of writing, Peel had the second highest concentration of COVID-19 cases in Ontario – 5,510 cases – accounting for 17% of the provincial cases [11].
On March 16, 2020, THP started screening and testing staff who reported symptoms in line with provincial recommendations. Between March 30 and May 27, THP also experienced 11 confirmed or presumptive outbreaks among patients and HCWs in a variety of hospital units. As part of investigating these outbreaks, the hospital offered testing to all HCWs working on those units in proximity to the outbreaks.
All symptomatic and asymptomatic HCWs testing positive during this period self-isolated for 14 days or longer.
Aligned with a new provincial mandate, on May 27, the hospital began a mass asymptomatic testing campaign of all asymptomatic clinical (physicians, nurses, allied health professionals) and non-clinical HCWs. All staff – whether working at the hospital or at home as a result of temporary closure of clinics and operating rooms – were strongly encouraged to receive a polymerase chain reaction (PCR) test [19], but testing was not mandatory. Specimens were collected with nasopharyngeal swabs (BD collection kit B220531), and nucleic acid extraction and amplification was performed on the BD MAX System (Becton Dickinson, Franklin Lakes, NJ) using the ExK TNA-2 kits. Real-time reverse transcription – PCR was run using a previously verified lab-developed test targeting the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) envelope (E gene), 5 ft. untranslated region, nucleocapsid gene, and human endogenous RNase P. Mass testing was offered at all hospital campuses over 20 consecutive days during work hours. HCWs working from home were notified of the availability of testing through email.
Testing was conducted in four risk waves relative to the HCW’s likelihood to care for or be in contact with COVID-19 patients. Screening for COVID-19 symptoms was conducted before each test performed during the campaign, aligned with the provincial ministry guidelines at the time. These symptoms included fever, new or worsening cough, shortness of breath, runny nose or nasal congestion, loss of the sense of taste or smell, sore throat or difficulty swallowing, nausea or vomiting, diarrhea, and abdominal pain. The highest risk group included physicians, nurses, and respiratory therapists working in emergency rooms, dedicated COVID-19 inpatient wards, and intensive care units, and the lowest risk group included corporate staff and those working virtually or off site. Employment records were used to classify individuals into these risk categories. See Appendix 1 for further details. Staff were encouraged to participate in the asymptomatic testing campaign, with repeated communications directly from the chief executive officer and daily rounding by front-line leaders to discuss and answer questions. Leaders met daily to discuss results and strategies to overcome barriers. Staff who tested positive were contacted by contact tracing staff with a standardized intake and self-isolation and contact tracing protocols.
Using SAS statistical software (version 9.4; SAS Institute, Cary, NC), z-tests were conducted to test for differences in proportions, and χ2 tests were used to test for differences in age distributions. Statistical significance was set at α = 0.05. Staff who received testing during the period from May 27 to June 15, 2020, because of symptoms (n = 449; 4.2%) are excluded from this analysis. No outbreaks and related testing occurred at the hospital during this period. This study was considered by THP’s Research Ethics Board to not be research.
RESULTS
Between March 27 and June 23, 2020, 5,204 (51.3%) of a total 10,143 hospital personnel were tested for COVID-19 by THP. This number includes 2,751 HCWs (27.1%) tested as part of the mass asymptomatic testing campaign conducted between May 27 and June 15, and 2,961 HCWs (29.2%) tested for symptoms or as a part of earlier outbreak investigations. Five hundred and eight HCWs (5.0%) who received a test during the mass asymptomatic testing campaign also received an earlier test in addition to this surveillance testing either because of symptoms or as part of an outbreak investigation.
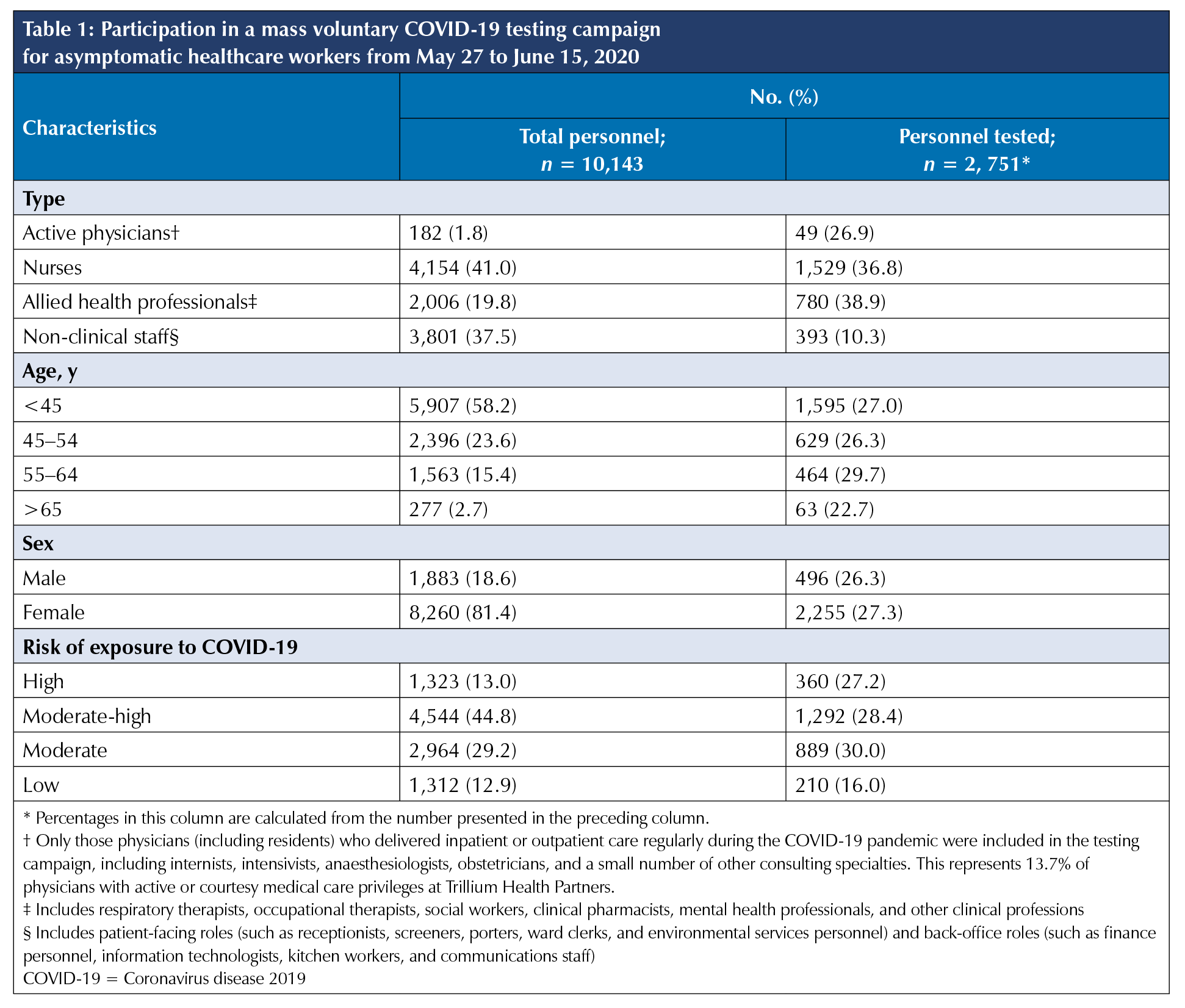
During the mass asymptomatic testing campaign for asymptomatic infection, 36.8% of nurses, 38.9% of allied health professionals, and 26.9% of active hospital physicians presented voluntarily for testing (Table 1). This was significantly greater than the 10.3% of non-clinical personnel presenting who worked in non–patient care areas, in corporate locations, or remotely at home (p < 0.0001). Among those who were tested, the likelihood of testing was significantly higher in the 55-64 age group – 29.7% versus 22.7% to 27.0% in the other age groups (p = 0.014). We found no significant difference in testing by sex (p = 0.401). When stratified by risk of exposure to COVID-19 patients in the hospital, similar proportions of personnel in high, moderate-high, and moderate risk areas presented for testing (27.2% to 30.0%); this combined percentage of 28.8% was significantly higher than the 16.0% of personnel with low likelihood of occupational exposure (p < 0.0001). The most common reported reasons for rejecting the offer of asymptomatic testing were at-home staff not wanting to come to the hospital for testing, fear of the nasopharyngeal swab, and having a previous negative test result.
During the asymptomatic testing campaign, 0.2% (5/2,751) individuals tested positive for COVID-19. This compares with 6.4% (188/2,961) positivity of THP personnel who were tested earlier because of symptoms or as a part of an outbreak investigation. Of the five individuals who tested positive, follow-up interviews revealed that two were symptomatic before the test, but did not self-identify at testing because of low awareness of mild symptoms. The remaining three individuals all subsequently developed mild symptoms of COVID-19, such as sore throat, runny nose, anosmia, ageusia, and fatigue. No secondary infections from these individuals were detected. Because of small numbers, we do not present breakdowns by job type, sex, age, or risk strata. During the mass testing period, the community of Peel reported 55 new cases per 100,000 and a community test positivity of 5% [20]. Before April 30, 9.2% of tests in the Peel region were positive [21].
DISCUSSION
In one large hospital system in one of Canada’s largest epicentres of COVID-19 infection, interest in voluntary testing was high, with more than half of hospital front-line and back-office personnel receiving at least one test during the 11-week period from March 30 to June 15. This included more than a quarter of personnel tested as part of an asymptomatic testing campaign to understand the prevalence of infection among asymptomatic staff. Clinical HCWs were more than three times more likely than non-clinical HCWs to present for asymptomatic testing, which may be due to a perceived greater risk for infection. The fact that we found no large differences in asymptomatic testing rates for clinical personnel working in areas of the hospital with different exposures to COVID-19 – positive patients may be because their perceived risk was in part modified by adequate supply and use of PPE and other infection control practices at the hospital during this time.
The low percentage of positivity for asymptomatic testing (0.2%) for HCWs during the campaign was somewhat expected, given that the percentage of positivity in the surrounding community was post-peak and was declining. This finding is also aligned with observations from Spain that showed that HCW infection rates mirrored community prevalence and may relate more to community than occupational exposure [9]. Our finding of no discernable differences in positivity among high- and
low-risk HCWs is also aligned with reports from others [13].
In contexts such as this in which community prevalence is declining and adequate PPE and other infection control practices are in place, healthcare decision makers should question the value of mass asymptomatic institutional testing campaigns. In the face of limited testing capacity and the opportunity costs related to such campaigns, it may be preferential to steward testing resources toward proactively testing segments of the community who may be experiencing higher infection rates or who are at higher risk to identify cases, contact trace, and isolate those who test positive. Mass asymptomatic testing may have more value in outbreak settings in which uncontrolled spread is suspected and in certain vulnerable populations, such as those living in congregate settings. For COVID-19 surveillance purposes in healthcare, more value may be attained from repeated sampling of HCWs who are continually exposed and at risk versus generalized testing strategies.
In summary, this article presents the results of one of the largest mass HCW testing strategies in Canada. These results are critical to report in order to understand the impact of unprecedented testing approaches. As further testing campaigns are rolled out across Canada, efforts should be made to systematically collect and summarize the findings in order to inform ongoing testing surveillance and pandemic control.
Contributors: Conceptualization, RJR; Methodology, NM; Formal Analysis, NM; Data Curation, NM; Writing – Original Draft, RJR; Writing – Review & Editing, LR, NM, LNS.
Ethics approval: This study was not considered research by Trillium Health Partners’ Research Ethics Board.
Informed consent: No informed consent was obtained because this study was considered not research. Personnel gave their consent to testing as anyone would for a clinical procedure.
Funding: The study was supported by Trillium Health Partners. Drs Reid and Rosella receive research salary support from the Trillium Health Partners Foundation and the Canada Research Chairs program, respectively.
Disclosures: All authors receive salary support from Trillium Health Partners, Trillium Health Partners Foundation, or both.
Peer review: This manuscript has been peer reviewed.
REFERENCES
1. World Health Organization. Coronavirus disease
(COVID-19) situation report—147. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200615-covid-19-sitrep-147.pdf?sfvrsn=2497a605_4 (Accessed June 15, 2020).
2. Dryhurst S, Schneider CR, Kerr J, et al. Risk perceptions of COVID-19 around the world. J Risk Res. 2020. (ePub Ahead of Print) https://doi.org/10.1080/13669877.2020.1758193
3. Angus Reid Institute. COVID-19 concern: half in Canada now worried about risk of infection among friends, family & community. http://angusreid.org/wp-content/uploads/2020/03/2020.03.10_coronavirus_pdf.pdf (Accessed June 16, 2020).
4. Simione L, Gnagnarella C. Differences between health workers and general population in risk perception, behaviors, and psychological distress related to COVID-19 spread in Italy. PsyArXiv. 2020. https://doi.org/10.31234/osf.io/84d2c.
5. Karasneh R, Al-Azzam S, Muflih S, Soudah O, Hawamdeh S, Khader Y. Media’s effect on shaping knowledge, awareness risk perceptions and communication practices of pandemic COVID-19 among pharmacists. Res Social Adm Pharm. 2020. (In Press) https://doi.org/10.1016/j.sapharm.2020.04.027. Medline: 32340892
6. Cai H, Tu B, Ma J, et al. Psychological impact and coping strategies of frontline medical staff in Hunan between January and March 2020 during the outbreak of coronavirus disease 2019 (COVID19) in Hubei, China. Med Sci Monit. 2020;26:e924171. https://doi.org/10.12659/MSM.924171.
7. Canadian Medical Association. CMA rapid poll on the supply of personal protective equipment. https://www.cma.ca/sites/default/files/pdf/Survey/CMA-Survey-Supply-of-PPE_E.pdf (Accessed June 16, 2020).
8. Barrett ES, Horton DB, Roy J, Gennaro ML, Brooks A, Tischfield J, et al. Prevalence of SARS-CoV-2 infection in previously undiagnosed health care workers at the onset of the U.S. COVID-19 epidemic. medRxiv. 2020. https://doi.org/10.1101/2020.04.20.20072470.
9. Folgueira MD, Munoz-Ruiperez C, Alonso-Lopez MA, Delgado R. SARS-CoV-2 infection in health care workers in a large public hospital in Madrid, Spain, during March 2020. medRxiv. 2020. https://doi.org/10.1101/2020.04.07.20055723.
10. Alberta Health Services. COVID-19 Scientific Advisory Group rapid response report. https://www. albertahealthservices.ca/assets/info/ppih/if-ppih-covid-19-hcw-risk-rapid-review.pdf (Accessed June 16, 2020).
11. Government of Ontario. Situation Report #140: COVID-19. Toronto: Ministry of Health, Health System Emergency Management Branch; 2020.
12. Ran L, Chen X, Wang Y, Wu W, Zhang L, Tan X. Risk factors of healthcare workers with corona virus disease 2019: a retrospective cohort study in a designated hospital of Wuhan in China. Clin Infect Dis. 2020. (In Press) https://doi.org/10.1093/cid/ciaa287. Medline: 32179890
13. Hunter E, Price DA, Murphy E, et al. First experience of COVID-19 screening of health-care workers in England. Lancet. 2020;395(10234):e77–e8. https://doi.org/10.1016/S0140-6736(20)30970-3.
14. Black JRM, Bailey C, Przewrocka J, Dijkstra KK, Swanton C. COVID-19: the case for health-care worker screening to prevent hospital transmission. Lancet. 2020;395(10234):1418–20. https://doi.org/10.1016/S0140-6736(20)30917-X.
15. Mertz D, Evans GA, Hota S. The pitfalls of mass hospital health care worker testing for COVID-19. JAMMI. 2020;5(3):121–3. https://doi.org/10.3138/jammi-2020-06-17.
16. Treibel TA, Manisty C, Burton M, et al. COVID-19: PCR screening of asymptomatic health-care workers at London hospital. Lancet. 2020;395(10237):1608–10. https://doi.org/10.1016/S0140-6736(20)31100-4.
17. Rivett L, Sridhar S, Sparkes D, et al. Screening of healthcare workers for SARS-CoV-2 highlights the role of asymptomatic carriage in COVID-19 transmission. Elife. 2020;9:e58728.
18. Public Health Agency of Canada. Coronavirus disease (COVID-19): Outbreak update. https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection.html?topic=tilelink#a1 (Accessed June 16, 2020).
19. Public Health Ontario. Coronavirus disease 2019 (COVID-19) testing. https://www.publichealthontario.ca/en/laboratory-services/test-information-index/wuhan-novel-coronavirus (Accessed June 16, 2020).
20. Region of Peel. Peel COVID-19 weekly epidemiological update—June 12 2020. https://www.peelregion.ca/health/professionals/pdfs/COVID-19/epi-update-20-12-06.pdf (Accessed June 29, 2020).
21. Chung H, Fung K, Ferreira-Legere LE, et al. COVID-19 laboratory testing in Ontario: patterns of testing and characteristics of individuals tested, as of April 30, 2020. Toronto: ICES; 2020.


