Carolyn Ingram, MPH1*, Mary Archibald, MPH1, Elizabeth Alvarez, MD, MPH, PhD2, Carla Perrotta, MD, MSc, PhD1
1School of Public Health, Physiotherapy, and Sports Sciences, University College Dublin, Belfield, Dublin 4, Ireland
2Department of Health Research Methods, Evidence and Impact, McMaster University, Hamilton, ON, Canada
*Corresponding author:
Carolyn Ingram
School of Public Health, Physiotherapy, and Sports Sciences
University College Dublin
Belfield, Dublin 4
Ireland
Tel: +33768304443 | email: This email address is being protected from spambots. You need JavaScript enabled to view it.
ABSTRACT
Background: Under the Occupational Health and Safety Act, every person employed in Canada has the right to a safe work environment. Yet, research shows that essential workers in Canada have experienced a disproportionate burden of COVID-19 transmission and deaths throughout the pandemic. In light of ongoing reported COVID-19 outbreaks in Canadian essential sectors and rising national case numbers as of July 2021, this study aimed to examine workers’ perceptions of the prevalence and effectiveness of occupational COVID-19 control measures during the fourth wave of the pandemic in Canada.
Methods: Individuals working on site in Canada from July 1 to November 30, 2021 were recruited through the Canadian Union of Public Employees (N=421). Data were collected on workplaces’ implementation of the COVID-19 Hierarchy of Controls. Adjusted odds ratios (AOR) and 95% confidence intervals (CI) generated from logistic regression models were used to estimate the likelihood of feeling protected at work vs. feeling unprotected or unsure according to participant characteristics and workplace control measures.
Results: The 421 respondents were predominantly female (75%, N=316), college-educated (63%, N=265), and in non-management roles (86%, N=364). Participants in education (AOR=0.4, 95% CI=0.2-0.9) or transportation/warehousing (AOR=0.3, 95% CI=0.1-0.9) were less likely to feel protected than those in healthcare. Ventilation adjustments (16%, N=66) and random or universal COVID-19 testing were rare (≤3%, N≤13), 40% (N=170) of participants’ workplaces used a contact tracing program. Employees adherence to physical distancing and masking requirements varied by occupational sector. Physical barriers (AOR=2.8, 95% CI=1.4-16.8), handwashing stations (AOR=4.8, 95% CI=1.4-16.8), testing of close contacts (AOR=2.1, 95% CI=1.2-3.7), and temperature checks (AOR=2.2, 95% CI=1.0-4.7) were associated with feeling protected at work after accounting for sector and managerial effect.
Conclusion: Limited COVID-19 controls were identified in transportation, manufacturing, warehousing, and education settings. Workers highlighted a need for improved ventilation, and upscaled asymptomatic screening, test and trace, and isolation efforts. Respondents’ uncertainty regarding the implementation of out-of-sight infection controls coupled with gaps in workers’ and scientists’ perceptions of effective safety measures indicate a need for improved communication strategies between occupational health experts, supervisors, and employees on pandemic risks and procedures.
KEYWORDS
infection control; COVID-19; workplace; Canada; frontline workers; Delta
INTRODUCTION
To combat workplace infectious disease outbreaks, the Canadian Centre for Occupational Health and Safety (CCOHS), in accordance with the World Health Organization (WHO), "advises that a layered approach to prevent and control occupational transmission of COVID-19 be determined and implemented following the Hierarchy of Controls [1], a system used to combine and deploy effective public health and occupational safety and health (OSH) controls within an organization [1, 2]. From most to least effective, recommended controls for all workplaces include eliminating the hazard by facilitating remote work when possible (Elimination); replacing the hazard with something less hazardous (Substitution); encouraging vaccination, improving ventilation, and installing physical barriers and hand hygiene equipment (Engineering controls); communicating rules and procedures, staggering shifts, screening and testing, disinfecting environmental surfaces, expanding access to sick leave (Administrative controls); and complementing other measures with the use of suitable and efficient personal protective equipment (PPE) [1, 2].
Under the Occupational Health and Safety Act, every person employed in Canada has the right to a safe work environment [3]. Yet, research shows that essential workers in Canada have experienced a disproportionate burden of COVID-19 transmission and deaths throughout the pandemic [4], and that sociodemographic inequalities in occupational risks of exposure driven by overrepresentation of women, immigrants, minority groups, and low-income workers in medium-to-high-risk industries (i.e., healthcare and social assistance, agriculture, food manufacturing, educational services, and transportation and warehousing) have left certain individuals at disproportionate risk of infection [5, 6]. Beyond physical risk, anxiety due to fear of contracting COVID-19 and infecting family members in conjunction with fear of the financial consequences of taking time off work can adversely affect frontline employees’
mental health [7]. Thus, improved worker protections in lower-paid, medium-to-high-risk occupational settings are needed to optimize the equity and effectiveness of Canada’s COVID-19 response.
Noting gaps concerning the prevalence and distribution of COVID-19 controls within Canadian workplaces continuing to operate during the pandemic, Smith et al. [8] examined the occupational control measures in place according to 53,316 employed respondents to Statistics Canada’s Labour Force Survey from July to September 2020 (this time period coincided with relatively low daily case counts in Canada). Generally high levels of workplace COVID-19 controls were identified, however, those working in the agricultural, construction, transportation, warehousing, and education industries identified fewer measures in place. In July 2021, to account for widespread vaccinations and in light of ongoing reported outbreaks in Canadian essential sectors and rising national case numbers [5], our research team sought to provide an update on the COVID-19 protections available to essential workers in Canada according to occupational sector. Using a validated online survey instrument, this study aimed to examine workers’ perceptions of the prevalence of occupational COVID-19 control measures during the fourth pandemic wave in Canada, and to assess how implemented measures related to feeling safe at work.
METHODS
Participants and study design
The sample comprised participants who were working part-time or full-time on site in Canada during the Delta-driven fourth wave of the pandemic (July 1 to November, 30 2021). Participants were recruited online through non-probability convenience sampling techniques. Of 12 geographically and occupationally representative OSH organizations and trade unions contacted by the researchers, three agreed to email the survey link to their constituents and/or post the survey link on their website: the Ontario Occupational Health Nurses Association (~400 members), BC General Employees’ Union (~3,600), and Canadian Union of Public Employees (~700,000). Eligibility criteria included: 1) aged 18 or over; and, 2) actively employed from July to November, 2021; and, 3) fluent in English, French, Spanish, Hindi, Polish, or Chinese. Participants working full-time from home were excluded from the study.
All data were collected using a validated, multilingual online questionnaire for surveying the COVID-19 prevention and control measures used in global workplaces [9]. Participants were given access to a study information sheet from the survey homepage. Informed consent to participate was requested before the survey could begin. The study’s procedures were reviewed and approved by the University College Dublin Human Research Ethics Committee (LS-E-21-138-Perrotta), and complied with the Declaration of Helsinki.
Control Measures
At the Elimination level, participants were asked if they were able to work part-time from home. As no measures for replacing the hazard with a non-hazardous substance have been identified, no questions were asked at the Substitution level. Participants were asked “Which of the following measures are currently in place in your workplace in response to COVID-19?” and instructed to select ‘Yes’, ‘No’, or ‘Unsure’ from the following recommended measures [1, 2]:
• Engineering controls: vaccination status, ventilation adjustments, air-quality monitoring, physical barriers, handwashing stations;
• Administrative controls: frequent disinfection of touched surfaces, COVID-19 signage, worker bubbles, facility entry restrictions, contact-tracing program, access to paid COVID-19 sick leave, COVID-19 testing of symptomatic, close contact, random groups, or all employees, self-isolation of symptomatic, close contact, or COVID-19-positive employees, and screening using temperature checks, or symptom reporting; and,
• PPE: masking requirement, training for use of PPE.
To assess adherence to administrative controls and PPE, participants were asked how often (1) they were able to maintain a 1-meter physical distance at work [10]; and, (2) masks were worn correctly by colleagues (response options: Never, Rarely, Sometimes, Always). Participants were also asked, “Do you feel protected from COVID-19 at work?” (response options: Yes, No, Unsure).
Data analysis
Participants’ occupations falling under the North American Industry Classification System (NAICS) were regrouped to balance for sample size:
• Office-based Trades/Services: Real estate or rental and leasing; finance or insurance; information and communication; professional, scientific, or technical services, administration, labour union.
• Outdoor Trades/Services: Mining and quarrying; construction; water supply; sewerage, waste management or remediation services; forestry, fishing, hunting or agriculture support; golf course maintenance.
• Retail Trades/Services: Accommodation or food services; retail trade; arts, entertainment, or recreation; health and fitness; cleaning activities.
• Public Administration: Public administration and defence; law enforcement; corrections.
• Transportation, Manufacturing: Transportation or warehousing; manufacturing and food processing.
• Healthcare: Doctor, nurse, laboratory technician working outside of hospital setting.
• Hospital: Healthcare professional working in hospital setting.
• Long-term care facility (LTCF): LTCF, assisted living facility.
• Social Services: social support worker, home visits.
• Educational Services: teacher at day care, primary, secondary, university level.
Chi square and Fisher Exact tests were performed to assess differences in implemented control measures according to occupation type. Odds ratios (OR) and adjusted odds ratios (AOR) generated from logistic regression models were used to estimate the likelihood of feeling protected at work vs. feeling unprotected or unsure according to participant characteristics and workplace control measures. Control measures responses were re-coded as Yes = 2, No or Uncertain = 1 for logistic regression analyses under the hypothesis that employees must be aware of control measures in place in order to feel protected by them. To account for multiple comparisons, a Bonferroni correction was applied during univariable analysis, and the significance threshold set at p <0.01. Variables emerging as significant were included in multivariable analysis, and stepwise descending selection by Akaike information criterion (AIC) performed to determine the best-fit multivariable model (significance level: p < 0.05). Participants for whom a certain response was missing were excluded from statistical test(s) involving that variable. Analysis was performed using R version 4.0.2. Maps of participant responses were rendered with the R Studio Leaflet package (R Foundation for Statistical Computing, Vienna, Austria).
Results
Participant Characteristics
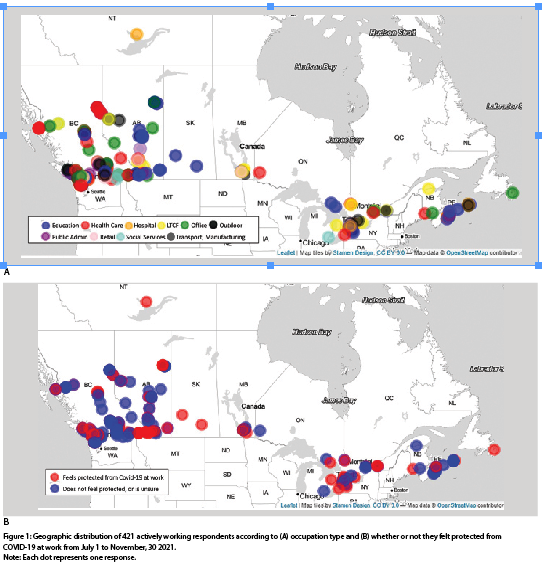
608 surveys were initiated in Canada, of which 187 were excluded from analysis due to missing occupational sector (N=59), incompletion (N=19), or because respondents worked full-time from home (N=100), or were not working at the time of data collection (N=9). Figure 1 shows the geographic range of survey responses yielding primarily from British Columbia, Alberta, Ontario, and Nova Scotia. At a glance, no geographic patterns emerged in respondent occupations or feeling protected at work. Respondents’ socio-demographic and occupational characteristics are displayed in Table 1. The 421 included respondents were predominantly female (75%, N=316), college-educated (63%, N=265), and in non-management roles (86%, N=364) at public institutions (68%, N=286).
Univariable logistic regression results for feeling protected at work vs. feeling unprotected or unsure are displayed in Table 1, and results from the adjusted model in Table 2. Working in a management role (AOR=2.9, 95% CI =1.1-7.9) significantly increased a participant’s likelihood of feeling protected from COVID-19 at work after adjustment for occupation type and multilevel control measures. Conversely, participants in education (AOR=0.4, 95% CI = 0.2-0.9) or transportation/warehousing (AOR=0.3, 95% = 0.1-0.9) were less likely to feel protected than those in healthcare.
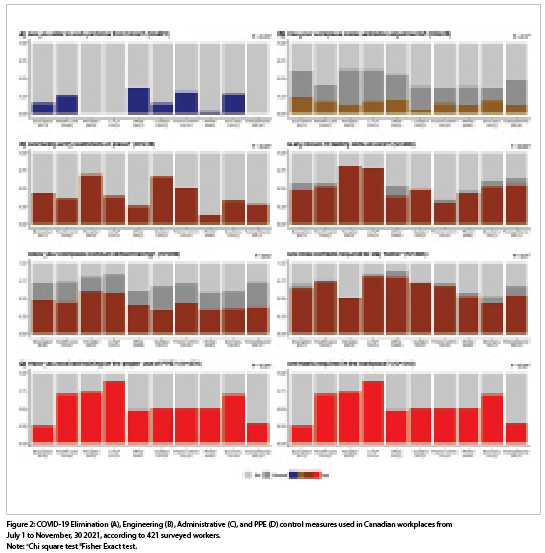
Elimination
A remote working option was unavailable to most participants (81%, N = 342) (Table 1) though this varied significantly by occupation type (p < 0.001, Figure 2). Working from home part-time did not significantly increase the likelihood of a participant feeling protected while on the job (OR=0.8, 99% CI=0.5-1.9).
Engineering Controls
Nearly all participants had received at least one dose of an approved COVID-19 vaccine (89%, N=329). Only two workers had not yet received access to a vaccine; 45 were unvaccinated by choice. Ventilation adjustments (16%, N=66) and air quality monitoring (5%, N=22) were rarely identified, whereas most participants reported handwashing stations (92%, N=388). Physical barriers (43%, N=179) were more present in office-based, public administration, and outdoor sectors than in healthcare settings, education, and transportation/manufacturing (p=0.008).
Physical barriers (AOR=2.8,95% CI=1.6-4.7) and handwashing stations (OR=4.8, 99% CI=1.4-17) significantly increased a participant’s likelihood of feeling protected at work after adjustment for occupation, rank, and administrative control measures.
Administrative Controls
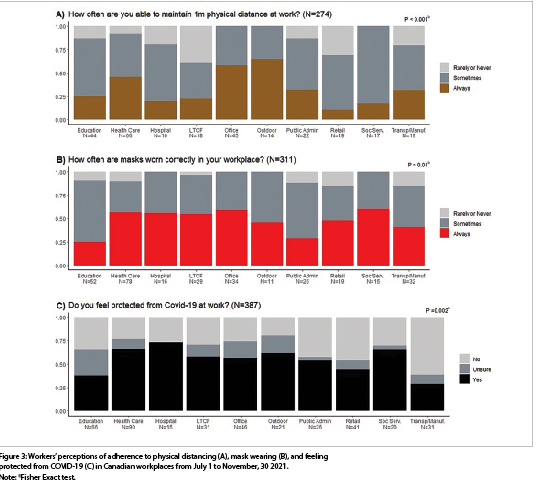
Most respondents reported disinfection procedures (84%, N=355) and use of COVID-19 signage (80%, N=337). By contrast, worker bubbles (23%, N=96) were not widely used, and facility entry restrictions varied by occupation (p <0.001, Figure 2). Physical distancing was more frequently adhered to in office- and outdoor-based settings than other occupational settings (p < 0.001, Figure 3).
Symptom reporting took place in half of participants’ workplaces (N=191). Temperature checks were indicated less frequently (18%, N=74). Less than 3% (N=13) of surveyed workers had undergone random or universal COVID-19 testing; approximately one third reported testing of symptomatic workers or close contacts. A majority of hospital and LTCF respondents had undergone some type of workplace testing, compared to a minority of those from non-healthcare settings (p = 0.003, Figure 2). Only 40% (N=170) of participants’ workplaces used a contact tracing program. Most employees had access to paid COVID-19 sick leave (59%, N=249) and/or were required to stay at home if a close contact (64%, N=268).
Worker bubbles, entry restrictions, testing and self-isolation of close contacts, temperature checks, symptom reporting, contact tracing, and adherence to physical distancing were all independently associated with feeling protected at work (Table 1). However, only the effects of testing close contacts (AOR=2.1, 95% CI = 1.2-3.7) and temperature checks (AOR=2.17, 95% CI = 1.0-4.7) remained significant in the adjusted model (Table 2). More ubiquitous measures such as COVID-19 signage and isolation requirements for symptomatic or COVID-19 positive workers were not associated with feeling protected at work.
PPE
Most respondents were required to wear masks at work (72%, N=302), particularly in healthcare-related or transport and manufacturing industries (p < 0.001, Figure 2). The provision of training for use of PPE varied significantly by occupational sector (p < 0.001), as did the frequency with which masks were worn correctly (p=0.01, Figure 3). Independent associations between masking use, adherence, and PPE training, and feeling protected at work were attenuated after adjustment for occupation, rank, and engineering/administrative controls.
One-third of respondents felt unprotected from COVID-19 at work (N=128) and 13% were unsure (N=53). In the transport/manufacturing, retail, and education sectors, these ratios were higher (p = 0.002, Figure 3).
DISCUSSION
Using a cross-sectional, online survey, this study examined frontline workers’ awareness of occupational COVID-19 control measures in place during the fourth-pandemic wave in Canada and how those measures related to risk perception. Results revealed sector-level differences in COVID-19 controls and feeling protected on the job. Respondents from non-healthcare occupations such as education, retail trades, and transportation/manufacturing systematically reported fewer controls in place and a greater sense of unprotection. Engineering controls, despite their increased effectiveness, were less frequently reported than administrative controls or PPE irrespective
of occupation. We believe this snapshot of workers’ perceptions calls to light several important considerations for Canada’s ongoing and future pandemic, occupational safety and health response.
First, according to workers, workplaces appear to have ‘gotten it right’ in many ways. COVID-19 control measures highlighted in national workplace health and safety guidance [1] including mask wearing, handwashing stations, isolation/quarantine, disinfection, and vaccination were used in most respondents’ workplaces. Workers in Canada reported a higher average number of occupational protective measures overall compared to individuals who took the same survey in China, Ireland, Argentina, and the UK [9]. Two-thirds of study participants felt protected from COVID-19 at work, particularly those in high-risk healthcare and hospital settings where outbreaks involving the Delta variant were reported during the study period [11]. Nevertheless, similar to results of the Statistics Canada’s Labour Force Survey conducted from July to September 2020 [8], workers identified persistent low levels of protections in transport, warehousing, manufacturing, and education settings one year later.
Engineering controls such as ventilation adjustments and air quality monitoring are critical for mitigating airborne transmission of SARS-CoV-2 in indoor settings, particularly in the context of the hyper-infectious Delta variant dominant at the time of data collection [12, 13]. Yet, only 16% of participants were aware of environmental adjustments having taken place in their workplace as of November 2021. The effectiveness of complementary measures like physical barriers depends on good ventilation [14]; indicating that for the 80 survey respondents whose workplaces reportedly had not made changes to ventilation but used physical barriers, the latter measure may have been doing little to redirect respiratory emissions at potential cost to employee health and to the company. Administrative controls were more widely reported and, encouragingly, symptom reporting and isolation strategies for symptomatic workers not uncommon. Yet, because a high proportion of Delta infections took place during the pre-symptomatic phase [15, 16], low reported rates of asymptomatic screening, testing and isolation measures coupled with limited use of contact tracing likely impeded the prevention and control of workplace outbreaks. Furthermore, the effectiveness of administrative controls and PPE depends on adherence to those controls. Despite the administrative changes reported and prevalence of masking requirements, a minority of respondents felt that physical distancing and mask wearing were correctly adhered to all of the time.
In some instances, workplaces may have implemented control measures unbeknownst to survey respondents. This is most plausible in the case of less visible engineering or administrative controls (30% of respondents marked ‘Unsure’ when asked if ventilation adjustments and contact tracing were used, though this could also indicate uncertainty regarding the definitions of these terms). Canada’s Occupational Health and Safety act entitles workers to know about and participate in health and safety decisions [3], and for good reason. If unapprised of safety measures in place, workers may experience anxiety based on overestimated perceived risk of contracting COVID-19. The 87 workers we surveyed who were unsure if they had access to paid COVID-19 sick leave may have been more inclined to come in to work if symptomatic or a close contact. Studies have also demonstrated positive associations between perceived risk of contracting COVID-19 at work and disengagement, turnover intention, burnout, and low morale amongst frontline employees [17]. In contrast, research indicates that strengthening formal and informal communication paths between supervisors and employees could encourage employee adherence to COVID-19 controls and reduce emotional exhaustion [18, 19]. As many respondents were unsure about their workplace’s application of out-of-sight control measures despite widely reported use of signage, more active communication tools and strategies (i.e., collaborative development, exploiting established informal communication-and-support networks of workers, solid orientation programs with education on safety measures and proper use of PPE) are an important consideration in Canada [20].
Improved OSH communications are also critical for addressing the gap identified in this study between workers’ and scientists’ perceptions of effective COVID-19 safety measures. Multivariable analysis revealed physical barriers, handwashing stations, testing of close contacts, and temperature checks as the measures most associated with feeling protected at work after accounting for sector and managerial effect. However, researchers have contested the sensitivity of temperature checks for SARS-CoV-2 detection and as previously noted, the effectiveness of physical barriers without appropriate ventilation and/or in settings with long-duration contacts [14, 21]. Alternatively, while “no-visitor” policies implemented in Canadian healthcare settings reduce SARS-CoV-2 transmission risk, they may have trickle-down consequences for employee mental health. The absence of family members or designated support persons who are important in the delivery of patient-centred care (e.g., feeding, mobility, emotional support) can, by increasing healthcare professionals’ workload, contribute to stress and burnout [22, 23]. These examples underline the importance of engaging with workers to identify effective, acceptable, and feasible OSH solutions; all the more so because vulnerable Canadian workers tend towards a “wait-and-see” approach when they have safety concerns [24], and because workers used to performing operations may unknowingly become acclimated to unacceptable risk over time [25].
This study, although meticulously conducted is not free of limitations. In this regard, it is important to note the potential for sample bias inherent to the non-probability convenience sampling techniques used. The viewpoints expressed by constituents of the Ontario Occupational Health Nurses Association, BC General Employees’ Union, and Canadian Union of Public Employees represented in this study may not be representative of frontline Canadian workers as a whole, particularly workers without the protections afforded by union membership. As well, small numbers due to lower survey uptake in non-healthcare settings required us to aggregate NAICS classifications, thereby preventing the reporting and interpreting of results by specific occupation. External validity may be impacted by the limited ability of an online survey instrument to capture viewpoints of workers with limited literacy skills and/or access to technology. Internal validity may be impacted by differences between workers perceptions of effective controls vs. empirical measures of effective controls (e.g., 111 workers surveyed on correct mask wearing had not received training on PPE use). Despite these limitations, this study serves as an important follow-up to the Statistics Canada’s 2020 Labour Force Survey [8] by demonstrating the ongoing need for improved COVID-19 control measures’ implementation and adherence in frontline occupational settings over one year into the COVID-19 pandemic.
CONCLUSION
Essential workers surveyed from July to November 2021 highlighted a need for improved ventilation, and upscaled asymptomatic screening, test and trace, and isolation efforts in high-to-medium risk occupational settings in Canada. Respondents’ uncertainty regarding the implementation of out-of-sight infection controls coupled with gaps in workers’ and scientists’ perceptions of effective safety measures indicate a need for improved communication strategies between occupational health experts, supervisors, and employees on pandemic risks and procedures.
REFERENCES
1. Canadian Centre for Occupational Health and Safety (CCOHS), Government of Canada. Take a Layered Approach to Control COVID-19 in the Workplace [Internet]. [cited 2022 May 5]. Available from: https://www.ccohs.ca/covid19/controls-infographic/index.html.
2. World Health Organization. Preventing and mitigating COVID-19 at work. Geneva; 2021 May. Available from: https://www.who.int/publications/i/item/WHO-2019-nCoV-workplace-actions-policy-brief-2021-1.
3. CCOHS, Government of Canada. OH&S Legislation in Canada – Three Rights of Workers : OSH Answers [Internet]. [cited 2022 May 5]. Available from: https://www.ccohs.ca/oshanswers/legisl/three_rights.html.
4. Rao, A., Ma, H., Moloney, G., Kwong, J.C., Jüni, P., Sander, B., et al. (2021). A disproportionate epidemic: COVID-19 cases and deaths among essential workers in Toronto, Canada. Annals of Epidemiology; 63:63–7.
5. Buchan, S.A., Smith, P.M., Warren, C., Murti, M., Mustard, C., Kim, J.H., et al. Incidence of outbreak-associated COVID-19 cases by industry in Ontario, Canada, 1 April 2020–31 March 2021. Occup Environ Med [Internet].[cited 2022 May 3]; Available from: https://oem.bmj.com/content/early/2022/01/11/oemed-2021-107879.
6. St-Denis, X. Sociodemographic Determinants of Occupational Risks of Exposure to COVID-19 in Canada (2020). Canadian Review of Sociology/Revue canadienne de sociologie;57(3):399–452.
7. Chen, Y., Ingram, C., Downey, V., Roe, M., Drummond, A., Sripaiboonkij, P., et al. Employee Mental Health During COVID-19 Adaptation: Observations of Occupational Safety and Health/Human Resource Professionals in Ireland. Int J Public Health [Internet]. 2022 [cited 2022 Aug 23];0. Available from: https://www.ssph-journal.org/articles/10.3389/ijph.2022.1604720/full.
8. Statistics Canada, Government of Canada. The prevalence and correlates of workplace infection control practices in Canada between July and September 2020 [Internet].[cited 2022 May 4]. Available from: https://www.doi.org/10.25318/82-003-x202101100002-eng.
9. Ingram, C., Chen Y., Buggy, C., Downey, V., Archibald, M., Rachwal, N., et al. (2022). Development and validation of a multi-lingual online questionnaire for surveying the COVID-19 prevention and control measures used in global workplaces. BMC Public Health; 22(1):74.
10. Chu, D.K., Akl, E.A., Duda, S., Solo, K., Yaacoub, S., Schünemann, H.J., et al. (2020). Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a
systematic review and meta-analysis. The Lancet; 395(10242):1973–87.
11. Susky, E.K., Hota, S., Armstrong, I.E., Mazzulli, T., Kestenberg, S., Casaubon, L.K., et al. (2021). Hospital outbreak of the severe acute respiratory coronavirus virus 2 (SARS-CoV-2) delta variant in partially and fully vaccinated patients and healthcare workers in Toronto, Canada. Infection Control & Hospital Epidemiology; 28:1–4.
12. Liu, Y., Liu J., Johnson, B.A., Xia, H., Ku, Z., Schindewolf, C., et al. (2022). Delta spike P681R mutation enhances SARS-CoV-2 fitness over Alpha variant. Cell Reports; 39(7):110829.
13. Saito, A., Irie, T., Suzuki, R., Maemura, T., Nasser, H., Uriu, K., et al. (2022). Enhanced fusogenicity and pathogenicity of SARS-CoV-2 Delta P681R mutation. Nature; 602(7896):300–6.
14. Eykelbosh, A. A rapid review of the use of physical barriers in non-clinical settings and COVID-19 transmission. [Internet].[cited 2022 May 04]. Available from: https://ncceh.ca/documents/evidence-review/rapid-review-use-physical-barriers-non-clinical-settings-and-covid-19.
15. Kang, M., Xin, H., Yuan, J., Ali, S.T., Liang, Z., Zhang, J., et al. (2022). Transmission dynamics and epidemiological characteristics of SARS-CoV-2 Delta variant infections in Guangdong, China, May to June 2021. Eurosurveillance; 27(10):2100815.
16. Hwang, H., Lim, J.S., Song, S.A., Achangwa, C., Sim, W., Kim, G., et al. (2022). Transmission Dynamics of the Delta Variant of SARS-CoV-2 Infections in South Korea. The Journal of Infectious Diseases; 225(5):793–9.
17. Moyo, N., Bhappu, A.D., Bhebhe, M., Ncube, F. (2022). Perceived Risk of COVID-19 and Employee Decision-Making: How Psychological Distress during the Pandemic Increases Negative Performance Outcomes among Healthcare Workers. International Journal of Environmental Research and Public Health; 19(11):6762.
18. Haas, E.J., Yorio, P.L. (2021). Behavioral safety compliance in an interdependent mining environment: supervisor communication, procedural justice and the mediating role of coworker communication. Int J Occup Saf Ergon;1–13.
19. Falco, A., Girardi, D., Corso, L.D., Yıldırım, M., Converso, D. (2021). The perceived risk of being infected at work: An application of the job demands–resources model to workplace safety during the COVID-19 outbreak. PLoS One; 16(9):e0257197.
20. Evia, C., Patriarca, A., (2012). Beyond Compliance: Participatory Translation of Safety Communication for Latino Construction Workers. Journal of Business and Technical Communication; 26(3):340–67.
21. Facente, S.N., Hunter, L.A., Packel, L.J., Li, Y., Harte, A., Nicolette. G., et al. (2021). Feasibility and effectiveness of daily temperature screening to detect COVID-19 in a prospective cohort at a large public university. BMC Public Health; 21(1):1693.
22. Brophy, J.T., Keith, M.M., Hurley, M., McArthur, J.E. (2021). Sacrificed: Ontario Healthcare Workers in the Time of COVID-19. New Solut; 30(4):267–81.
23. Munshi, L., Evans, G., Razak, F. (2021). The case for relaxing no-visitor policies in hospitals during the ongoing COVID-19 pandemic. CMAJ; 193(4):E135–7.
24. Tucker, S., Turner, N. (2013). Waiting for safety: Responses by young Canadian workers to unsafe work. Journal of Safety Research; 45:103–10.
25. Naji, G.M.A., Isha, A.S.N., Alazzani, A., Saleem, M.S., Alzoraiki, M. Assessing the Mediating Role of Safety Communication Between Safety Culture and Employees Safety Performance. Frontiers in Public Health [Internet]. [cited 2022 May 5];10. Available from: https://www.frontiersin.org/article/10.3389/fpubh.2022.840281.


